Wildlife, ecology and the next pandemic
Sign over I-93 in Boston warning of COVID-19 travel restrictions in Massachusetts
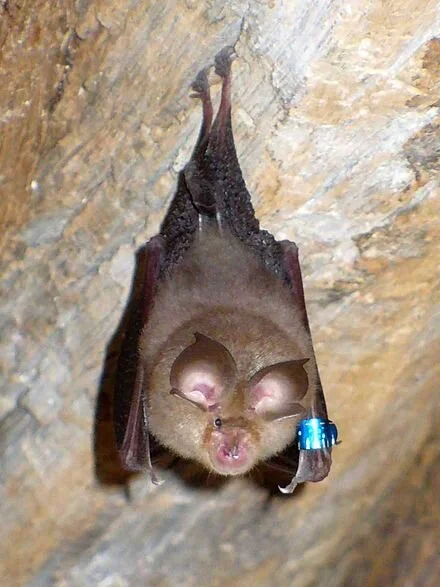
A horseshoe bat, seen as likely source of COVID-19
As the COVID-19 pandemic heads for a showdown with vaccines it’s expected to lose, many experts in the field of emerging infectious diseases are already focused on preventing the next one.
They fear another virus will leap from wildlife into humans, one that is far more lethal but spreads as easily as SARS-CoV-2, the strain of coronavirus that causes COVID-19. A virus like that could change the trajectory of life on the planet, experts say.
“What keeps me up at night is that another coronavirus like MERS, which has a much, much higher mortality rate, becomes as transmissible as covid,” said Christian Walzer, executive director of health at the Wildlife Conservation Society. “The logistics and the psychological trauma of that would be unbearable.”
SARS-CoV-2 has an average mortality rate of less than 1%, while the mortality rate for Middle East respiratory syndrome, or MERS — which spread from camels into humans — is 35%. Other viruses that have leapt the species barrier to humans, such as bat-borne Nipah, have a mortality rate as high as 75%.
“There is a huge diversity of viruses in nature, and there is the possibility that one has the Goldilocks characteristics of pre-symptomatic transmission with a high fatality rate,” said Raina Plowright, a virus researcher at the Bozeman Disease Ecology Lab, in Montana. (COVID-19 is highly transmissible before the onset of symptoms but fortunately is far less lethal than several other known viruses.) “It would change civilization.”
That’s why in November the German Federal Foreign Office and the Wildlife Conservation Society held a virtual conference called One Planet, One Health, One Future, aimed at heading off the next pandemic by helping world leaders understand that killer viruses like SARS-CoV-2 — and many other less deadly pathogens — are unleashed on the world by the destruction of nature.
With the world’s attention gripped by the spread of the coronavirus, infectious disease experts are redoubling their efforts to show the robust connection between the health of nature, wildlife and humans. It is a concept known as One Health.
While the idea is widely accepted by health officials, many governments have not factored it into policies. So the conference was timed to coincide with the meeting of the world’s economic superpowers, the G20, to urge them to recognize the threat that wildlife-borne pandemics pose, not only to people but also to the global economy.
The Wildlife Conservation Society — America’s oldest conservation organization, founded in 1895 — has joined with 20 other leading conservation groups to ask government leaders “to prioritize protection of highly intact forests and other ecosystems, and work in particular to end commercial wildlife trade and markets for human consumption as well as all illegal and unsustainable wildlife trade,” they said in a recent press release.
Experts predict it would cost about $700 billion to institute these and other measures, according to the Wildlife Conservation Society. On the other hand, it’s estimated that covid-19 has cost $26 trillion in economic damage. Moreover, the solution offered by those campaigning for One Health goals would also mitigate the effects of climate change and the loss of biodiversity.
The growing invasion of natural environments as the global population soars makes another deadly pandemic a matter of when, not if, experts say — and it could be far worse than covid. The spillover of animal, or zoonotic, viruses into humans causes some 75% of emerging infectious diseases.
But multitudes of unknown viruses, some possibly highly pathogenic, dwell in wildlife around the world. Infectious disease experts estimate there are 1.67 million viruses in nature; only about 4,000 have been identified.
SARS-CoV-2 likely originated in horseshoe bats in China and then passed to humans, perhaps through an intermediary host, such as the pangolin — a scaly animal that is widely hunted and eaten.
While the source of SARS-CoV-2 is uncertain, the animal-to-human pathway for other viral epidemics, including Ebola, Nipah and MERS, is known. Viruses that have been circulating among and mutating in wildlife, especially bats, which are numerous around the world and highly mobile, jump into humans, where they find a receptive immune system and spark a deadly infectious disease outbreak.
“We’ve penetrated deeper into eco-zones we’ve not occupied before,” said Dennis Carroll, a veteran emerging infectious disease expert with the U.S. Agency for International Development. He is setting up the Global Virome Project to catalog viruses in wildlife in order to predict which ones might ignite the next pandemic. “The poster child for that is the extractive industry — oil and gas and minerals, and the expansion of agriculture, especially cattle. That’s the biggest predictor of where you’ll see spillover.”
When these things happened a century ago, he said, the person who contracted the disease likely died there. “Now an infected person can be on a plane to Paris or New York before they know they have it,” he said.
Meat consumption is also growing, and that has meant either more domestic livestock raised in cleared forest or “bush meat” — wild animals. Both can lead to spillover. The AIDS virus, it’s believed, came from wild chimpanzees in central Africa that were hunted for food.
One case study for how viruses emerge from nature to become an epidemic is the Nipah virus.
Nipah is named after the village in Malaysia where it was first identified in the late 1990s. The symptoms are brain swelling, headaches, a stiff neck, vomiting, dizziness and coma. It is extremely deadly, with as much as a 75% mortality rate in humans, compared with less than 1% for SARS-CoV-2. Because the virus never became highly transmissible among humans, it has killed just 300 people in some 60 outbreaks.
One critical characteristic kept Nipah from becoming widespread. “The viral load of Nipah, the amount of virus someone has in their body, increases over time” and is most infectious at the time of death, said the Bozeman lab’s Plowright, who has studied Nipah and Hendra. (They are not coronaviruses, but henipaviruses.) “With SARS-CoV-2, your viral load peaks before you develop symptoms, so you are going to work and interacting with your family before you know you are sick.”
If an unknown virus as deadly as Nipah but as transmissible as SARS-CoV-2 before an infection was known were to leap from an animal into humans, the results would be devastating.
Plowright has also studied the physiology and immunology of viruses in bats and the causes of spillover. “We see spillover events because of stresses placed on the bats from loss of habitat and climatic change,” she said. “That’s when they get drawn into human areas.” In the case of Nipah, fruit bats drawn to orchards near pig farms passed the virus on to the pigs and then humans.
“It’s associated with a lack of food,” she said. “If bats were feeding in native forests and able to nomadically move across the landscape to source the foods they need, away from humans, we wouldn’t see spillover.”
A growing understanding of ecological changes as the source of many illnesses is behind the campaign to raise awareness of One Health.
One Health policies are expanding in places where there are likely human pathogens in wildlife or domestic animals. Doctors, veterinarians, anthropologists, wildlife biologists and others are being trained and training others to provide sentinel capabilities to recognize these diseases if they emerge.
The scale of preventive efforts is far smaller than the threat posed by these pathogens, though, experts say. They need buy-in from governments to recognize the problem and to factor the cost of possible epidemics or pandemics into development.
“A road will facilitate a transport of goods and people and create economic incentive,” said Walzer, of the Wildlife Conservation Society. “But it will also provide an interface where people interact and there’s a higher chance of spillover. These kinds of costs have never been considered in the past. And that needs to change.”
The One Health approach also advocates for the large-scale protection of nature in areas of high biodiversity where spillover is a risk.
Joshua Rosenthal, an expert in global health with the Fogarty International Center at the National Institutes of Health, said that while these ideas are conceptually sound, it is an extremely difficult task. “These things are all managed by different agencies and ministries in different countries with different interests, and getting them on the same page is challenging,” he said.
Researchers say the clock is ticking. “We have high human population densities, high livestock densities, high rates of deforestation — and these things are bringing bats and people into closer contact,” Plowright said. “We are rolling the dice faster and faster and more and more often. It’s really quite simple.”
Jill Richardson: How do we get skeptics to get COVID shots?
U.S. airman Ramón Colón-López receives Pfizer COVID-19 vaccine at Walter Reed National Military Medical Center this month.
Via OtherWords.org
With the new COVID-19 vaccine available, Dr. Anthony Fauci says Americans can begin to achieve herd immunity by next summer. Herd immunity occurs when so many people are immune to the virus that it can’t spread, because an infected person won’t have anyone left to spread it to.
Yet as of last month, four in ten Americans said they definitely or probably won’t get the vaccine (although about half of that group said they would consider it once a vaccine became available and they could get more information about it).
Why, after living in quarantine for almost 10 months while the economy and our mental health crashes around us, after over 300,000 Americans are dead, is getting the vaccine even a question?
There are two ways to approach this question. The first is to dismiss it: Call vaccine skeptics derogatory names, post memes on social media about how stupid they are, and make rules requiring the vaccine.
The second way to approach the question is to try to understand vaccine skepticism in order to address Americans’ concerns.
Sociologist Jennifer Reich tied vaccine refusal to messages that treat health like a personal project, in which consumers must exercise their own discretion, and a culture of individualism in a world where there is not enough of anything to go around — jobs, money, health care, etc.
In this view, everyone must look out for themselves so they can get ahead, and that’s more important than doing your part to achieve herd immunity for our collective wellbeing.
Reich’s research on anti-vaxxers comes from before the current pandemic. She studied parents who refused to vaccinate their children for preventable diseases like measles. But it’s still worth considering in this new context. Reich believes it is unsurprising that some people do treat vaccines like a consumer choice and disregard that when they decline a vaccine, they endanger others too.
Another take on COVID vaccine refusal comes from Zakiya Whatley and Titilayo Shodiya, who are both women of color with PhDs in natural sciences. They focus on Black, Latinx and indigenous communities, who often distrust doctors. Their suspicion is not unfounded, given how much racism in medicine has harmed people of color, historically and in the present.
Scientists hold the power to define what is true and what is not in a way that non-scientists do not. Consider the power relations within medicine: When a patient goes to the doctor because they are ill, the doctor assesses their symptoms, makes a diagnosis, and prescribes a treatment.
Scientists determine what is recognized as a diagnosis and which treatments are available. Powerful financial interests (like pharmaceutical and insurance companies) play a major role too. The patient’s power is more limited: they can look up their symptoms on WebMD, accept or refuse the treatment prescribed, or go to a different doctor.
Sometimes lay people react to being on the less powerful end of the relationship by simply refusing to believe scientists. They might resist by embracing conspiracy theories or “barstool biology” that uses the language of science but not the scientific method.
Natural scientists have done their part by creating vaccines that are safe and highly effective. To get people to take the vaccine, we need social science. We must learn how to rebuild trust with people who have lost it. And we will do that by listening to them and understanding them, not by calling them stupid.
Jill Richardson, a sociologist, is an OtherWords.org columnist.
Headquarters of a COVID-19 vaccine inventor and maker, Moderna, in Cambridge, Mass. Greater Boston is one of the world’s centers of biotechnology.
New study says mask-wearing most important factor in cutting chance of getting COVID-19 during air travel
A Delta Airlines plane being disinfected between flights
From The New England Council (newenglandcouncil.com)
BOSTON
“Researchers at the Harvard T.H. Chan School of Public Health have completed a comprehensive, gate-to-gate study on how to greatly reduce the chances of COVID-19 transmission during air travel.
“The study concludes that universal mask-wearing, rigorous cleaning protocols and high-end air filtration systems lower the risk of COVID-19 transmission to minimal levels. The study found that mask-wearing among passengers and crew is the most important factor in reducing risk during air travel. The researchers also found that the use of high-efficiency particulate air (HEPA) filters is extremely effective in removing harmful airborne particles. Ultimately, diligently engaging in this multi-layered approach results in a substantially lowered risk of COVID-19 transmission during air travel in comparison to other activities.
“‘The risk of COVID-19 transmission onboard aircraft [is] below that of other routine activities during the pandemic, such as grocery shopping or eating out,’ the Harvard researchers concluded. 'Implementing these layered risk mitigation strategies…requires passenger and airline compliance [but] will help to ensure that air travel is as safe or substantially safer than the routine activities people undertake during these times.’
“Read more from the National Preparedness Initiative report.’’
Linda Gasparello: What’s good for us can be very bad for wildlife
Remains of an albatross killed by ingesting plastic pollution.
WEST WARWICK, R.I.
When I lived in Manhattan, I pursued an unusual pastime. I started it to avoid eye contact with Unification Church members who peddled flowers and their faith on many street corners in the 1970s. If a Moonie (as a church member was derisively known) were to approach me, I’d cast my eyes down to the sidewalk, where I’d see things that would set my mind wandering.
In the winter, I’d see lone gloves and mittens. On the curb in front of La Cote Basque on East 55th Street, the luxe French restaurant where Truman Capote dined with the doyennes of New York’s social scene, before dishing on them in his unfinished novel, Answered Prayers, I saw a black leather glove with a gold metal “F” sewn on the cuff. I coveted such a Fendi pair, eyeing them at the glove counter at Bergdorf Goodman, but not buying them – they cost about a third of my Greenwich Village studio apartment’s monthly rent in the late 1970s. On the sidewalk on Fifth Avenue, in front of an FAO Schwartz window, I saw a child’s mitten, expertly knit in a red-and-white Norwegian pattern that I never had the patience to follow. I wondered whether the child dropped the mitten after removing it to point excitedly to a toy in the window.
In the summer, I’d see pairs of sunglasses and single sneakers on the sidewalks, things that had fallen out of weekenders’ pockets and bags. It wasn’t unusual for me to see pantyhose. Working women in Manhattan, in my time there, could wear a short-sleeved wrap dress – the one designed by Diane von Furstenberg was the working woman’s boilersuit -- in the summer, but they’d better have put on pantyhose, or packed a pair in their pocketbooks or tote bags. The pantyhose would fall out of them and roll like tumbleweed along the avenues.
One summer morning on Perry Street, near where I lived, I saw a long, black zipper. It looked like a black snake had slithered out of a drain grate on the street and was warming itself on the asphalt, its white belly gleaming in the sun.
Now when I walk on a city sidewalk, I still look down, not to pursue my pastime but to preserve myself from tripping and falling on stuff. I sometimes see interesting litter, but mostly I see single-use and reusable face masks.
This fall, as I walked on the waterfront promenade along Rondout Creek in Kingston, N.Y., I saw a single-use mask swirling in the wind with the fallen leaves. I grabbed the mask and deposited it in a trash can, worried that it would fall into the creek, ensnarling the waterfowl and the fish.
In the COVID-19 crisis, masks have been lifesavers. But masks, especially single-use, polypropylene surgical masks, have been killing marine wildlife and devastating ecosystems.
Billions of masks have been entering our oceans and washing onto our beaches when they are tossed aside, where waste-management systems are inadequate or nonexistent, or when these systems become overwhelmed because of increased volumes of waste.
A new report from OceansAsia, a Hong Kong-based marine conservation organization, estimates that 1.56 billion masks will have entered the oceans in 2020. This will result in an additional 4,680 to 6,240 metric tons of marine plastic pollution, says the report, entitled “Masks on the Beach: The impact of COVID-19 on Marine Plastic Pollution.”
Single-use masks are made from a variety of meltdown plastics and are difficult to recycle, due to both composition and risk of contamination and infection, the report points out. These masks will take as long as 450 years to break down, slowly turning into microplastics ingested by wildlife.
“Marine plastic pollution is devastating our oceans. Plastic pollution kills an estimated 100,000 marine mammals and turtles, over a million seabirds, and even greater numbers of fish, invertebrates and other animals each year. It also negatively impacts fisheries and the tourism industry and costs the global economy an estimated $13 billion per year,” according to Gary Stokes, operations director of OceansAsia.
The report recommends that people wear reusable masks, and to dispose of all masks properly.
I hope that everyone will wear them for the sake of their own and others’ health, and that I won’t see them lying on sidewalks on my strolls, or on beaches, where they are a sorry sight.
Linda Gasparello is co-host and producer of White House Chronicle, on PBS. Her email is whchronicle@gmail.com and she’s based in Rhode Island and Washington, D.C.
Victoria Knight: Those tough COVID Christmas travel decisions
Our Lady of the Airways Chapel .at Logan International Airport, in Boston. You’d think that it would get crowded these days, given the new risks of travel. The chapel is the oldest airport chapel in the United States, opening originally in 1951 in another part of the airport.
Vivek Kaliraman, who lives in Los Angeles, has celebrated every Christmas since 2002 with his best friend, who lives in Houston. But, this year, instead of boarding an airplane, which felt too risky during the COVID pandemic, he took a car and plans to stay with his friend for several weeks.
The trip — a 24-hour drive — was too much for one day, though, so Kaliraman called seven hotels in Las Cruces, N.M. — which is about halfway — to ask how many rooms they were filling and what their cleaning and food-delivery protocols were.
“I would call at nighttime and talk to one front desk person and then call again at daytime,” said Kaliraman, 51, a digital health entrepreneur. “I would make sure the two different front desk people I talked to gave the same answer.”
Once he arrived at the hotel he’d chosen, he asked for a room that had been unoccupied the night before. And even though it got cold that night, he left the window open.
Scary Statistics Trigger Strict Precautions
Many Americans, like Kaliraman, who did ultimately make it to Houston, are still planning to travel for the December holidays, despite the nation’s worsening coronavirus numbers.
Last week, the Centers for Disease Control and Prevention reported that the weekly COVID hospitalization rate was at its highest point since the beginning of the pandemic. More than 283,000 Americans have died of COVID-19. Public health officials are bracing for an additional surge in cases resulting from the millions who, despite CDC advice, traveled home for Thanksgiving, including the 9 million who passed through airports Nov. 20-29. Hospital wards are quickly reaching capacity. In light of all this, health experts are again urging Americans to stay home for the holidays.
For many, though, travel comes down to a risk-benefit analysis.
According to David Ropeik, author of the book How Risky Is It, Really? and an expert in risk perception psychology, it’s important to remember that what’s at stake in this type of situation cannot be exactly quantified.
Our brains perceive risk by looking at the facts of the threat — in this case, contracting or transmitting COVID-19 — and then at the context of our own lives, which often involves emotions, he said. If you personally know someone who died of COVID-19, that’s an added emotional context. If you want to attend a wedding of loved family members, that’s another kind of context.
“Think about it like a seesaw. On one side are all the facts about COVID-19, like the number of deaths,” said Ropeik. “And then on the other side are all the emotional factors. Holidays are a huge weight on the emotional side of that seesaw.”
The people we interviewed for this story said they understand the risk involved. And their reasons for going home differed. Kaliraman likened his journey to see his friend as an important ritual — he hasn’t missed this visit in 19 years.
What’s clear is that many aren’t making the decision to travel lightly.
For Annette Olson, 56, the risk of flying from Washington, D.C., to Tyler, Texas, felt worth it because she needed to help take care of her elderly parents over the holidays.
“In my calculations, I would be less of a risk to them than for them to get a rotating nurse that comes to the house, who has probably worked somewhere else as well and is repeatedly coming and going,” said Olson. “Once I’m here, I’m quarantined.”
Now that she’s with her parents, she’s wearing a mask in common areas of the house until she gets her COVID test results back.
Others plan on quarantining for several weeks before seeing family members — even if, as in Chelsea Toledo’s situation, the family she hopes to see is only an hour’s drive away.
Toledo, 35, lives in Clarkston, Ga., and works from home. She pulled her 6-year-old daughter out of her in-person learning program after Thanksgiving, in hopes of seeing her mom and stepdad over Christmas. They plan to quarantine for several weeks and get groceries delivered so they won’t be exposed to others before the trip. But whether Toledo goes through with it is still up in the air, and may change based on COVID case rates in their area.
“We’re taking things week by week, or really day by day,” said Toledo. “There is not a plan to see my mom; there is a hope to see my mom.”
And for young adults without families of their own, seeing parents at the holidays feels like a needed mood booster after a difficult year. Rebecca, a 27-year-old who lives in Washington, D.C., drove up with a roommate to New York City to see her parents and grandfather for Hanukkah. (Rebecca asked KHN not to publish her last name because she feared that publicity could negatively affect her job, which is in public health.)
“I’m doing fine, but I think having something to look forward to is really useful. I didn’t want to cancel my trip completely,” said Rebecca. “I’m the only child and grandchild who doesn’t have children. I can control my actions and exposures more than anyone else can.”
She and her two roommates quarantined for two weeks before the drive and also got tested for COVID-19 twice during that time. Now that Rebecca is in New York, she’s also quarantining alone for 10 days and getting tested again before she sees her family.
“I think, based on what I’ve done, it does feel safe,” said Rebecca. “I know the safest thing to do is not to see them, so I do feel a little bit nervous about that.”
But the best-laid plan can still go awry. Tests can return false-negative results and relatives may overlook possible exposure or not buy into the seriousness of the situation. To better understand the potential consequences of the risk you’re taking, Ropeik advises coming up with “personal, visceral” thoughts of the worst thing that could happen.
“Envision Grandma getting sick and dying” or “Grandma in bed and in the hospital and not being able to visit her,” said Ropeik. That will balance the positive emotional pull of the holidays and help you to make a more grounded decision.
Harm Reduction?
All of those interviewed for this story acknowledged that many of the precautions they’re taking are possible only because they enjoy certain privileges, including the ability to work from home, isolate or get groceries delivered — options that may not be available to many, including essential workers and those with low incomes.
Still, Americans are bound to travel over the December holidays. And much like teaching safe-sex practices in schools rather than an abstinence-only approach, it’s important to give out risk mitigation strategies so that “if you’re going to do it, you think about how to do it safely,” said Dr. Iahn Gonsenhauser, chief quality and patient safety officer at the Ohio State University Wexner Medical Center.
First, Gonsenhauser advises that you look at the COVID case numbers in your area, consider whether you are traveling from a higher-risk community to a lower-risk community, and talk to family members about the risks. Also, check whether the state you’re traveling to has quarantine or testing requirements you need to adhere to when you arrive.
Also, make sure you quarantine before your trip — recommendations range from seven to 14 days.
Another thing to remember, Gonsenhauser said, is that a negative COVID test before traveling is not a free pass, and it works only if done in combination with the quarantine period.
Consider your mode of transportation as well — driving is safer than flying.
Finally, once you’ve arrived at your destination, prepare for what might be the most difficult part: to continue physical distancing, wearing masks and washing your hands. “It’s easy to let our guard down during the holidays, but you need to stay vigilant,” said Gonsenhauser.
Victoria Knight is a Kaiser Health News reporter
vknight@kff.org, @victoriaregisk
Llewellyn King: The traitorous tribe that kills fellow Americans
President Trump touring a Honeywell mask factory (!) in May 2020. As at many other crowded events he has attended during the pandemic, Trump and his entourage, (fearful of his rebuke) refused to wear masks at this highly publicized visit.
WEST WARWICK, R.I.
When a nation goes to war its first step to survival is to protect the homeland against invasion. Every citizen is co-opted: It is their national duty.
We are on a war footing against COVID-19. It has invaded our homeland, and it is slaughtering us. Nearly 300,000 are dead and the vast hospital network in the United States is overwhelmed.
A dark cloud passes before our sun. Christmas promises more sorrow as we wait for reinforcements -- in this case, the vaccine -- to arrive.
The first line of defense against this common enemy, this indiscriminate killer, is a simple piece of layered cloth or paper held over the nose and mouth by cloth or elastic strings. It is a face mask, the simplest of defensive weapons.
But there is in the United States a tribe that has lost its head, reminiscent of Nicholas Monserrat’s great novel of 1956, The Tribe That Lost Its head. (See an old cover below.)
There are among us those who won’t defend their homeland, won’t wear masks, and accompany that treason by propagating a theory that to wear a mask is to grant a malign government total authority over the individual, and to bring about totalitarianism; or that to wear a mask is to cede manhood or endanger our way of life.
Worse, there are those who believe that it is a political statement of solidarity with the outgoing administration, with the embattled president, and the raucous nationalism that is the core of his appeal.
Some won’t wear masks out of youthful chutzpah, believing this is a disease of the old and that the young and the healthy are immune. This is a fiction they have been fed by those who should know better and most likely do know better, most of whom reside under Republican roofs, presided over by that Niagara Falls of disinformation, President Trump.
While the nation is taking fatal casualties which it doesn’t need to take, while first responders and medical personal are thrown again and again into the breach, exhausted and scared, the Trump Republicans can’t bring themselves to join the battle.
While the signs of war — a war with a terrible count in deaths -- rages on, congressional Republicans are foraging for scandals like pigs after truffles. Most of them still won’t condemn Trump for his super-spreader activities, like his rallies, parties and reckless behavior in public, which signal masks aren’t needed.
The trouble is that leaders of this headless tribe, this unacceptable face of what was the Grand Old Party, are so cowed that they won’t check the president.
The Republican Party used to be made up of muscular individuals, lawmakers who took their mandate seriously, not today’s pusillanimous followers. Incredibly, most Republican members of Congress can’t bring themselves to admit that Joe Biden won the election and will be the next president. Had there been “massive voter fraud” this wouldn’t be so. The courts would have spoken other than as they have.
All of this has played into the anti-mask movement and its lethal consequences. The virus doesn’t ask party affiliation: It is an equal-opportunity slayer.
Then there is Trump’s great enabler in the Senate, Majority Leader Mitch McConnell.
Even as millions of Americans don’t know where the next meal will come from this Christmas besides a food bank, and rent and utility bills are unpaid, McConnell, and McConnell alone, will decide who gets relief, who gets the shaft for Christmas. He can just refuse to bring a bill to the floor and end it right there. His personal concerns are paramount, not those of the other members of Congress.
Not only does McConnell not wish to understand the gravity of the situation in the country, but he also seems to relish his ability to exacerbate it, to turn his job into a Lego game for his own amusement.
This will be a bleak Christmas lit by the hope that the vaccine will deliver us from despair and bottomless hurt.
But for the vaccine to vanquish the virus, we must get our shots. If the same idiocy that shuns masks prevails, the war won’t fully be won for years when it could be ended next year.
The sight of victory is the best Christmas present, and it is possible next year if we close ranks. Those who will bear the guilt are known. They are in Washington now.
Llewellyn King is executive producer and host of White House Chronicle, on PBS. His email is llewellynking1@gmail.com and he’s based in Rhode Island and Washington, D.C.
Web Site: whchronicle.com
John O. Harney: Update on college news in New England
At Wheaton College, which has done very well in facing COVID-19. Left to right: Emerson Hall, Larcom Hall, Park Hall, Mary Lyon Hall, Knapton Hall and Cole Chapel.
BOSTON
From The New England Journal of Higher Education, a service of The New England Board of Higher Education (nebhe.org)
Faculty diversity. In the early 1990s, NEBHE, the Southern Regional Education Board (SREB) and the Western Interstate Commission for Higher Education (WICHE) collaborated to develop the first Compact for Faculty Diversity. Formally launched in 1994, with support from the Ford Foundation and Pew Charitable Trust, the compact focused on five key strategies: motivating states and universities to increase financial support for minorities in doctoral programs; increasing institutional support packages to include multiyear fellowships, along with research and teaching assistantships to promote integration into academic departments and doctoral completion; incentivizing academic departments to create supportive environments for minority students through mentorship; sponsoring an annual institute to build support networks and promote teaching ability; and building collaborations for student recruitment to graduate study. With reduced foundation support, collaboration among the three participating regional education compacts declined, but some core compact activities continued through SREB.
Now, NEBHE and its sister regional compacts are launching a collaborative, nine-month planning process to reinvigorate and expand a national Compact for Faculty Diversity. Under the proposed new compact, NEBHE, the Midwestern Higher Education Compact (MHEC), SREB and WICHE would collaborate to invest in the achievement of diversity, equity and inclusion in faculty and staff at postsecondary institutions in all 50 states. Ansley Abraham, the founding director of the SREB State Doctoral Scholars Program at the SREB, has been instrumental in the design and execution of that initiative. He recently published this short piece in Inside Higher Ed.
Fighting COVID. As the head of the Centers for Disease Control and Prevention (CDC) warned of the roughest winter in U.S. public-health history, Wheaton College has stood out. Our Wheaton, in Norton, Mass. (not to be confused with the Wheaton College in Illinois) developed a plan based on science that has kept positive cases low on campus and allowed in-person classes during the fall semester. Wheaton was able to limit the college’s overall fall semester case count to 23 (a .06 positivity rate among 35,000 tests) due to strong protocols, rigorous testing through the Cambridge, Mass.-based Broad Institute and a shared commitment from the community, especially students. In early November, as cases were spiking across the U.S., the private liberal arts college had its own spike of 13 positive cases in one day. But thanks to immediate contact tracing in partnership with the Massachusetts Community Tracing Collaborative, only one positive case resulted after that day, notes President Dennis Hanno. Part of Wheaton’s success owes to its twice-a-week testing throughout the semester. The college also credits its work with the for-profit In-House Physicians to complement internal staff in managing on-campus testing and quarantine/isolation housing.
New England in D.C. The COVID-19 crisis should make national health positions crucial. Earlier this week, President-elect Joe Biden tapped Dr. Rochelle Walensky, an infectious disease physician at Medical School and Massachusetts General Hospital, to lead the CDC and Dr. Vivek Murthy, who attended Harvard and Yale and did his residency at Brigham and Women’s Hospital, to be surgeon general. They’ll work with Dr. Anthony Fauci, the chief medical advisor and College of the Holy Cross graduate who has served six presidents.
Last month, as Biden’s transition team began drawing on the nation’s colleges and universities to prepare to take the reins of government, we flashed back to a 2009 NEJHE piece when Barack Obama was stocking his first administration. “As they form their White House brain trusts, new presidents tend to mine two places for talent: their home states and New England—especially New England’s universities, and especially Harvard,” we noted at the time. Most recently, two New England Congresswomen have scored big promotions on Capitol Hill. Rosa DeLauro (D.-Conn.) became Appropriations chair and Katherine Clark (D.-Mass.) was elected assistant speaker of the House. Richard Neal (D.-Mass.) was already chairman of the powerful House Ways and Means Committee.
Indebted. U.S. Sen. Elizabeth Warren (D.-Mass.), long a champion of canceling student debt, called on Biden to take executive action to cancel student loan debt. “All on his own, President-elect Biden will have the ability to administratively cancel billions of dollars in student loan debt using the authority that Congress has already given to the secretary of education,” she told a Senate Banking Committee hearing. “This is the single most effective economic stimulus that is available through executive action.” About 43 million Americans have a combined total of $1.5 trillion in federal student loan debt. Such debt has been shown to discourage big purchases, growth of new businesses and rates of home ownership among other life milestones. Warren has outlined a plan in which Biden can cancel up to $50,000 in federal student loan debt for borrowers.
Jobless recovery? Everyone knew the public health crisis would be accompanied by an economic crisis. This week, Moody’s Investors Service projected that the 2021 outlook for the U.S. higher-education sector remains negative, as the coronavirus pandemic continues to threaten enrollment and revenue streams. The sector’s operating revenue will decline by 5 percent to 10 percent over the next year, Moody’s projected. The pace of economic recovery remains uncertain, and some universities have issued or refinanced debt to bolster liquidity. (As this biting piece notes, “Just as decreased state funding has caused students to go into debt to cover tuition and fees, universities have taken on debt to keep their doors open.”)
The name of the game for many higher education institutions (HEIs) is coronavirus relief money from the federal government. NEBHE has written letters to Congress calling for increased relief based on the many New England students and families struggling with reduced incomes or job loss and the costs associated with resuming classes that were significantly higher than anticipated. These costs have been growing based on regular virus testing, contact tracing, health monitoring, quarantining, building reconfigurations, expanded health services, intensified cleaning and the ongoing transition to virtual learning. Citing data from the National Student Clearinghouse, NEBHE estimated that New England’s institutions in all sectors lost tuition and fee revenue of $413 million. And that’s counting only revenue from tuition and fees. Most institutions also face additional budget shortfalls due to lost auxiliary revenues (namely, from room and board) and the high costs of compliance with new health regulations and the administration of COVID-19 tests to students, faculty and staff. (When the relief money is spent and by whom is important too. Tom Brady’s sports performance company snagged a Paycheck Protection Program loan of $960,855 in April.) Anna Brown, an economist at Emsi, told our friends at the Boston Business Journal that higher-ed staffers working in dorms, maintenance roles, housing and food services have been hit hard, and faculty will not be far behind
Admissions blast from the past. I’ve overheard too many conversations lately with reference to “testing” and wondered if the subject was COVID testing or interminable academic exams. Given admissions tests being de-emphasized by colleges, we were reminded me of a 10-year-old piece by Tufts University officials on how novel admissions questions would move applicants to flaunt their creativity. The authors told of how “Admissions officers use Kaleidoscope, as well as the other traditional elements of the application, to rate each applicant on one or more of four scales: wise thinking, analytical thinking, practical thinking and creative thinking.” Could be their moment?
Anti-wokism. The U.S. Department of Education held “What is to be Done? Confronting a Culture of Censorship on Campus” on Dec. 8 (presumably not deliberately on the anniversary of John Lennon’s assassination). The hook was to unveil the department’s “Free Speech Hotline” to take complaints of campus violations. The event organizers contended that “Due to strong demand, the event capacity has been increased!” The department’s Assistant Secretary for Postsecondary Education Robert King began noting that we’ll hear from “victims of cancel culture’s pernicious compact” where generally “administrators cave to the mob and punish the culprit.” He noted, “Coming just behind this are Communist-style re-education camps” and assured the audience that the department has launched several investigations into these kinds of offenses like those that land awkwardly in my inbox from Campus Reform. Universities are no place for “wokism,” one speaker warned, adding that calls for diversity and tolerance actually aim to squelch unpopular opinions.
Welcome dreamers. Last week, a federal judge ordered the Trump administration to restore the Deferred Action for Childhood Arrivals (DACA) program to how it was before the administration announced plans to end it in September 2017. DACA provides protection against deportation and work authorization to certain undocumented immigrants who were brought to the U.S. as children. DACA participants include many current and former college students. NEBHE issued a statement in support of DACA in September 2017 and has advocated for the initiative’s support.
John O. Harney is executive editor of The New England Journal of Higher Education.
David Warsh: A great victory in vaccine making and marketing
U.S. Government Accountability Office diagram comparing a traditional vaccine-development timeline to an expedited one
SOMERVILLE, Mass.
I often struggle to explain why I consider the Financial Times the best newspaper that I read. But my conviction begins with the consideration that the FT shows for my time and attention, as if it expects I have other things to do (in my case also reading The New York Times, The Washington Post and The Wall Street Journal). There are no “jumps,” all stories in the daily report end on the page where they begin. The front page displays just two stories (along with many teases of stories elsewhere in the paper); then come three pages of general news from around the world, followed by several pages of company and markets news; two pages of market data set in small type; a page of arts criticism, a full-page story (“The Big Read”); an editorial and letters page with four columns opposite, and, of course, the second most widely read page of the section, the “Lex” column of edgy newsy tidbits on the back. It is a thrifty package.
My deeper admiration, however, has to do to with the news values that the paper displays throughout. Last week presented a prime example. It takes a good deal of self-confidence to run out a story under the headline, “Trump vaccine chief proves critics wrong on Warp Speed: Industry veteran navigated political hurdles to boost drug companies’ fight against virus.”
But reporters Hannah Kuchler and Kiran Stacey had delivered a persuasive story. Since the article itself remains behind the FT paywall, I quote more extensively than I might otherwise to convey the gist. They began:
Sitting in the shadow of the brutalist health department building in Washington, with only a leather jacket for protection against an autumnal breeze, Moncef Slaoui cuts a defiant figure. Six months after the former GlaxoSmithKline executive left the private sector to become President Donald Trump’s coronavirus vaccine tsar, Mr Slaoui feels his decision has been vindicated, and critics of the ability of Operation Warp Speed to develop a vaccine in record time have been proved wrong.
“The easy answer for experts was to say it was impossible and find reasons why the operation would never work,” he told the Financial Times. But the vaccine push is now hailed as the bright spot in the Trump administration’s Covid-19 response, as products from Pfizer and BioNTech, Moderna, and AstraZeneca and Oxford university move closer to approval.
The next day, Karen Weintraub, of USA Today, produced an in-depth profile of Slaoui, a Moroccan-born Belgian-American vaccine developer and retired drug company executive. It is fascinating reading. But the authority of the FT account derived from the three experts the reporters quoted zeroing in on the management tool that Slaoui used to achieve his results, known as advance market commitments. or AMCs (and from a little Reuters sidebar that listed some of the spending on pre-approved doses by the U.S. government’s Biomedical Advanced Research and Development Authority (BARDA):
The central achievement of Operation Warp Speed had been accelerating investment in manufacturing, said Angela Rasmussen, a virologist at the Columbia University School of Public Health. “Normally, that would be a huge investment for a vaccine manufacturer to make, and potentially be a huge loss for them if they developed a vaccine that never went on to the market,” she said.
Even Pfizer, which did not take direct investment from Operation Warp Speed, benefited from having a $2bn pre-order for when its vaccine gets approved, said Peter Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering. “Even if J&J or someone else beat them to the punch, they were going to get paid,” he said.
Stéphane Bancel, chief executive of Moderna, the lossmaking biotech which took about $2.5bn in government funding from different bodies, said the money was “very helpful”, covering the costs of trials and helping it to buy raw materials. “The entire planet is going to benefit from it,” he told the FT. “We are going to file [for approval] in the UK based on the US data paid for by the US government. We’re going to file in Europe and hopefully have a vaccine available in France and Spain and Italy, all paid for by the US government.”
Part of the charm of the story turns on its rarity; it hadn’t been easy for mainstream media to find nice things to say about the Trump administration. The road to Slaoui’s hiring probably leads back to Vice President Mike’s Pence’s appointment in February as head of the White House Coronavirus Task Force. As former governor of Indiana, Pence’s connections with the pharmaceutical industry are tight; Indianapolis is home to major firms, including Eli Lilly and Purdue Pharma. Much remains to be learned.
But the mechanism known as advanced market commitment is of comparatively recent origin. It is the discovery, if that is the word, of University of Chicago economist Michael Kremer, in a series of papers he wrote while teaching at the Massachusetts Institute of Technology and Harvard University some 20 years ago, culminating in the publication, in 2004, of Strong Medicine: Creating Incentives for Pharmaceutical Research on Neglected Diseases, with his wife, Rachel Glennerster, in 2004.
The new mechanisms they advocated were similar to those that in the 18th Century gave rise to the development of the naval chronometer, necessary to determining longitude at sea. Governmental “pull” methods could complement the inherently risky “push” of private research and development. AMCs – legally binding commitments to buy specified quantities of as yet unavailable vaccines at specified prices – were the most promising of the lot for bringing into existence medicines that otherwise might not pay. I wrote in 2004 that the general line of argument of the book was “one more example of why, more than ever, governments today need talented and sophisticated regulators. Technology policy has become as important as monetary policy – in some respects, maybe more so.” (I am told that governmentally guaranteed long-term purchase contracts were the backbone of creating the Indonesia-Japan LNG trade, and developing so-called private power generation in the U.S.)
I asked Kremer last week if he had been involved in the Warp Speed journey, The answer was no. He and co-authors had spoken to staff at the Council of Economic Advisers in the run-up to the creation of Operation Warp Speed. They had co-authored an op-ed article in The New York Times last May. But they had not met with Slaoui. He seems to have imbibed the basic idea as long ago as 2013, when he organized a session on the industry’s stock of common knowledge for the Aspen Ideas festival
Kremer was recognized with a Nobel Prize in economics, with two others, in 2018, for work on policy evaluation, including the work on vaccines. But I was struck when Wall Street Journal editorial-page columnist Daniel Henninger suggested last week that the scientists at the pharmaceutical companies who developed vaccines against COVID-19 were “the obvious recipient for 2021’s Nobel Peace Prize.”
There’s no doubt that we owe a considerable debt of gratitude to the scientists. But it was the administration’s Operation Warp Speed that organized their successful quests. A Peace Prize for the swift development of vaccines is a very good idea, not for President Trump or for Vice President Pence, nor even, to make a needed point, for Moncef Slaoui. It is a pretty thought, but remember that Russian and Chinese scientists also produced vaccines. Let the Norwegian parliament figure it out!
David Warsh, an economic historian and a veteran columnist, is proprietor of Somerville-based economicprincipals.com, where this column first appeared.
Chris Powell: Running empty trains won't increase production; some people seem to be enjoying their pandemic lockdowns
— Photo by Chianti
MANCHESTER, Conn.
While Connecticut Gov. Ned Lamont remarked the other day that state government doesn't have enough money to rescue every business suffering from COVID-19 pandemic, most people think that the federal government has infinite money and can and should make everyone whole.
Sharing that view, Connecticut U.S. Sen. Richard Blumenthal this week went to the railroad station in West Haven to join Catherine Rinaldi, president of the Metropolitan Transit Authority, in calling for an emergency $12 billion federal appropriation for the MTA, which runs the Metro-North commuter railroad line from New Haven to New York City. Metro-North has lost 80 percent of its passengers and fares because of business curtailments and the shift to working from home.
There are two problems with the appeal from Blumenthal and Rinaldi.
First, there is no need to keep Metro-North operating on a normal schedule when most passengers are missing. Except for railroad employees, no one is served by running empty trains.
Indeed, curtailment of commuter-rail service might make time to renovate the tracks and other facilities. Rather than furloughing railroad employees, hundreds of them might be reassigned temporarily to collect the trash that litters the tracks between New Haven and New York. The savings on electric power from running fewer trains still would be huge.
The second problem is that the federal government's power of money creation is infinite only technically. While nothing in law forbids the federal government from spending any amount, money is no good by itself. It has value only insofar as it has purchasing power -- only insofar as there are things to be purchased, only insofar as there is production and with so many people out of work or working less during the epidemic, production has fallen measurably. Operating empty trains won't increase production, but spending $12 billion to operate them may worsen the devaluation of the dollar, whose international value recently has fallen substantially amid so much money creation.
So it might be far better to add that $12 billion to public-health purposes.
The $12 billion desired by the MTA is only a tiny part of the largess imagined by the incoming national administration and many members of Congress who will be returning to Washington next month. They are contemplating another trillion dollars in bailouts, and that's just for starters. Such is the damage done to the national economy by the epidemic and government's often clumsy responses to it.
“Scene in club lounge,’’ by Thomas Rowlandson (1757-1827)
Amid all the seemingly free money, some people are starting to enjoy lockdowns or at least finding them tolerable, especially those who, like many government employees, get paid as usual whether they work or not.
This week two Hartford City Council members, Wildaliz Bermudez and Josh Mitchtom, called on the governor to use the state's $3 billion emergency reserve to pay everybody to stay home for a month and to stop most commercial operations in the name of slowing the spread of the virus. Bermudez and Mitchtom seemed unaware that the emergency reserve is already expected to be consumed by the huge deficits pending in next year's state budget. The reserve won't come close to covering all the shortfalls.
But then getting paid for doing or accomplishing nothing is a way of life in Hartford, encouraged by state government's steady subsidy of so many failures in the city.
Last week a group of 35 doctors went almost as far as those Hartford council members, urging the governor to close gyms and restaurants and to prohibit all “unnecessary” gatherings so as to stop the virus and prevent medical personnel from being overwhelmed. It didn't seem to bother the doctors that those businesses and their employees already have been overwhelmed by commerce-curtailment orders, suffering enormous losses, including business capital and life savings. The doctors are inconvenienced now and may be more so but they won't be losing their life savings and livelihoods.
The governor is trying to strike a balance among all these interests. Every day presents him with another difficult judgment call that upsets someone. He may be realizing that Connecticut is just going to have to tough it out and accept some casualties all around.
Chris Powell is a columnist for the Journal Inquirer, in Manchester.
Llewellyn King: COVID-19 points way to faster medicines
In a Food and Drug Administration lab in Silver Spring, Md.
WEST WARWICK, R.I.
This is the month when the national spirit should start to lift: COVID-19 vaccines could be administered by mid-December. While we won’t reach the summit of a mighty mountain this month, nor well into next year, the ascent will have begun.
It is unlikely to be a smooth journey. There will be contention, accusation, litigation and frustration. Nothing so big as setting out to administer two-dose vaccines to the whole country could be otherwise.
But the pall that hangs so heavily over us with rising deaths, exhausted first responders and overstretched hospitals, will begin to lift very slightly.
For the rest of foreseeable history, there will be accusations leveled at the Trump administration for its handling of the pandemic — or its failure to handle it.
But one thing is certain: Our faith in our ability to make superhuman scientific efforts in the face of crisis will be restored. Developing a COVID-19 vaccine will be compared to putting a man on the Moon.
The large pharmaceutical companies, known collectively as Big Pharma, have shown their muscle. The lesson: Throw enough research and unlimited money at a problem, accelerate the regulatory process, and a solution can result.
Even globalization gets a good grade.
The first-to-market vaccine comes from American pharmaceutical giant Pfizer. But the vaccine was developed at its small German subsidiary, BioNTech, by a husband-and-wife team of first-generation Turkish immigrants. (Beware of whom you exclude.)
Biopharmaceutical research often takes place this way, akin to how it happens in Silicon Valley: Small companies innovate and invent, and larger ones gobble them up and provide the all-important resources for absurdly complicated and expensive clinical trials. These contribute mightily to the cost of new drugs. A new “compound” -- as a drug is called in the trade -- can cost up to $2 billion to bring to market; and financial reserves are needed, should there be costly lawsuits.
The development of new drugs looks like an inverted pyramid. Linda Marban, a researcher and CEO of Capricor Therapeutics Inc., a clinical-stage biotechnology company based in Los Angeles, explained it to me: “The last 20 years have shown a seismic change in how drugs and therapies are developed. Due to the speed at which science is advancing, and the difficulty of early-stage development, most of the early-stage work is done by small companies or the occasional academic. Big Pharma has moved into the role of late-stage clinical, sometimes Phase 2, but mostly Phase 3 and commercial development.”
In the upheaval occasioned by the pandemic, overhaul of the Food and Drug Administration looms large as a national priority. It must be able -- maybe with a greater use of artificial intelligence and data management -- to assess the safety and efficiency of desperately needed drugs without the current painful and often fatal delays.
Marban said of the FDA clinical-trials process: “It is the most laborious and frustrating process which delays important scientific and medical discoveries from patients. There are many situations where patients are desperate for therapy, but we have to climb the long and ridiculous ladder of doing clinical trials due to inefficiencies at the site which include nearly endless layers of contracting, budget negotiations, IRB [Institutional Review Board] approvals and, finally, interest and attention from overworked clinical trial staff.”
This situation, according to Marban, is compounded by the FDA’s requirement for clinical trials conducted and presented in a certain way, which often precludes getting an effective therapy to market. “If we simplify this process alone, we could move rapidly towards treatments and even cures for many horrific diseases,” she added.
War is a time of upheaval, and we are at war against the COVID-19. But war also involves innovation. We have proved that speed is possible when bureaucracy is energized and streamlined.
When COVID-19 is finally vanquished, it should leave a legacy of better medical research and sped-up approval procedures, benefiting all going forward.
Llewellyn King is executive producer and host of White House Chronicle, on PBS. His email is llewellynking1@gmail.com and he’s based in Rhode Island and Washington, D.C.
Linda Gasparello
Co-host and Producer
"White House Chronicle" on PBS
Mobile: (202) 441-2703
Websi
Janie Grice: For an essential workers' bill of rights
From OtherWords.org
During the pandemic, essential workers have become public heroes. These frontline workers include tens of millions of retail employees, from those who stock our grocery shelves to those filling orders for Amazon.
With so many people seeing firsthand how low-wage workers make our society function, we have a once-in-a-lifetime opportunity to transform our society so that everyone can earn quality pay and benefits.
But beyond symbolic displays of gratitude, essential retail workers have not yet seen this transformation.
At Walmart, the largest private employer in the country, workers are still not receiving adequate hazard pay, safety protections or paid leave. The company remains the top employer of workers who are forced to rely on food stamps and other aid.
At Amazon, employees still face rigid limits on bathroom breaks and other policies that compromise their health and safety in the midst of a pandemic. At least 20,000 Amazon employees have tested positive for COVID-19.
These issues are deeply personal to me.
For four years, I worked at my local Walmart as a cashier and later as a customer-service manager — all while raising my son as a single mother and working on a bachelor’s degree. I started out making only $7.78 an hour and was never able to get a full-time position, let alone a stable schedule.
I understand the stresses faced by retail workers at our country’s largest employers, including struggling to pay bills and not being able to care for a sick child because of unpredictable hours and low wages.
Despite the challenges of the job, I got my degree in social work and now support retail workers across the country as an organizer for United for Respect. This national organization of working people fights for bold policies that would improve lives, particularly those in the retail industry.
One of our priority goals is an Essential Workers Bill of Rights, which would guarantee improved health and safety protections, universal health care, increased pay and paid leave, and whistleblower protection.
Workers also need a real voice in policy matters that affect our lives, from union organizing rights to personal protective equipment. So we’re pushing to get worker representation on corporate boards.
Without these rights, corporate executives and politicians will continue to put their interests before those of essential workers and their families. And retail workers, especially Black women like me, will continue to live in poverty while working for some of the largest and wealthiest employers in the world.
During the pandemic, the wealth of Amazon CEO Jeff Bezos and Walmart’s Walton family has skyrocketed to record levels, according to a new report by Bargaining for the Common Good, the Institute for Policy Studies, and United for Respect. The contrast between this wealth and the struggles essential workers face is shameful.
If this nation wants a real conversation about dignity for people like me and the people I organize, then we have to embrace bold solutions. And we can start with an Essential Workers Bill of Rights and a voice for workers in decision making.
Think about what corporate America would look like if workers actually had a seat at the table. Corporations would prioritize investments in their workers instead of padding their CEOs’ pockets. The millions of retail workers who now have to rely on food stamps and other public assistance could provide for their families.
Let’s push toward this dream by expanding opportunities for the working people who are critical to the health and security of our nation — today, during the pandemic, and beyond.
Janie Grice is an organizer with United for Respect, based in Marion, S.C.
— Photo by Lars Frantzen
Ed Cervone: How a Maine college has adjusted to pandemic and recession
From The New England Journal of Higher Education, a service of The New England Board of Higher Education (nebhe.org)
In October 2019, NEBHE called together a group of economists and higher education leaders for a meeting at the Federal Reserve Bank of Boston to discuss the future of higher education (Preparing for Another Recession?). No one suspected that just months later, a global pandemic would turn the world upside down. Today, the same challenges highlighted at the meeting persist. The pandemic has only amplified the situation and accelerated the timeline. It also has forced the hands of institutions to advance some of the changes that will sustain higher education institutions through this crisis and beyond.
At the October 2019 meeting, the panelists identified the primary challenges facing colleges and universities: a declining pool of traditional-aged students, mounting student debt, increasing student-loan-default rates and growing income inequality.
Taken together, these trends were creating a perfect storm, simultaneously putting a college education out of reach for more and more students and forcing some New England higher-education institutions to close or merge with other institutions. Those trends were expected to continue.
Just three months later, COVID-19 had begun spreading across the U.S., and the education system had to shut down in-person learning. Students returned home to finish the semester. Higher-education institutions were forced to go fully remote in a matter of weeks. Institutions struggled to deliver content and keep students engaged. Inequities across the system were accentuated, as many students faced connectivity obstacles. Households felt the economic crunch as the unemployment rate increased sharply.
By summer, the pandemic was in full swing. Higher-education institutions looked to the fall. They had to convince students and their families that it would be safe to return to campus in an uncertain and potentially dangerous environment. Safety measures introduced new budgetary challenges: physical infrastructure upgrades, PPE and the development of screening and testing regimens.
In the fall, students resumed their education through combinations of remote and in-person instruction. Activities and engagement looked very different due to health and safety protocols. Many institutions experienced a larger than usual summer melt due to concerns from students and families about COVID and the college experience.
Despite these added challenges, New England higher-education institutions have adapted to keep students engaged in their education, but are running on small margins and expending unbudgeted funds to continue operations during the public-health crisis. Recruiting the next class of students is proving to be a challenge. The shrinking pool of recruits will contract even more and reaching them is much more difficult. Many low- and moderate-income families will find accessing higher education even harder and may choose to defer postsecondary learning.
Change is difficult but a crisis can provide necessary motivation. Maine institutions are using this opportunity to make the changes needed to address the current crisis that will also set them on a more sustainable path over the long term. Maine has a competitive advantage relative to the nation. A low-density rural setting and the comprehensive public-health response from Gov. Janet Mills have kept the overall incidence rate down. Public and private higher-education institutions coordinated their response, developed a set of protocols for resuming in-person education that were reviewed by the governor and public health officials, and successfully returned to in-person education in the fall.
In addition, Mills established the Economic Recovery Committee in May and charged the panel with identifying actions and investments that would be necessary to get the Maine economy back on track. This public process has reinforced the critical ties between education and a healthy economy. Not only is higher education a focus of the work, but the governor appointed Thomas College President Laurie Lachance to co-chair the effort. In addition, the governor appointed University of New England (in Biddeford, Maine) President James Herbert, University of Maine at Augusta President Rebecca Wyke, and Southern Maine Community College President Joseph Cassidy to serve on the committee.
At the individual institution level, a wide array of innovations will enable Thomas College to endure the pandemic and position itself for the future. Consider:
Affordability. Most Thomas College students come from low- to medium-income households and are the first in their families to attend college, so-called “first-generation” students. Cost will always be top of mind. For motivated students, Thomas has an accelerated pathway that allows students to earn their bachelor’s degree in three years (sometimes two) and they have the option of doing a plus-one to earn their master’s. This, coupled with generous merit scholarship packages (up to $72,000 of scholarship over four years) and a significant transition to Open Educational Resources to reduce book costs, represents real savings and the opportunity to be earning sooner than their peers.
Student success supports. Accelerated programs (or any program, for that matter) are not viable without purposeful strategies to keep students on track to complete based on their plans. In addition to a traditional array of academic and financial supports, Thomas College has invested in a true wraparound offering serving the whole student. For eligible students, Thomas has a dedicated TRIO Student Support Services program. Funded through a U.S. Department of Education grant, the program provides academic and personal support to students who are first-generation, are from families of modest incomes, or who have an identified disability. The benefits include individualized academic coaching, financial literacy development and college planning support for families. Thomas was also first in the nation to have a College Success program through JMG (Maine’s Jobs for America’s Graduates affiliate). Thomas College has expanded physical- and mental- health services in the wake of the pandemic, including our innovative Get Out And Live program, which uses Maine’s vast natural setting to provide a range of exciting four-season, outdoor activities for the whole campus community.
Employability. Thomas College students see preparing for a rewarding career as part of their college experience. This is core to the college’s mission and more important than ever in an uncertain economic environment. It is so important that it is guaranteed through the college’s Guaranteed Job Program. Thomas College’s Centers of Innovation focus on the employability of each student. Students pursue a core academic experience in their chosen field, and staff work with each student starting in their first semester to increase their professional and career development. This means field experiences and internships with Maine’s top employers. About 75 percent of Thomas College students have an internship before graduation. As part of their college experience, Thomas College students are coached to earn professional certificates, licenses and digital badges prior to graduation that make them stand out in their professional fields and improve their earning potential. These might include certificates in specific sectors like accounting and real estate or digital badges that show proficiency in professional skills like Design Thinking or Project Management, to name just a few. On the academic side, Thomas has expanded both undergraduate and graduate degree offerings to programs where the market has great demand, including Cybersecurity, Business Analytics, Applied Math, Project Management and Digital Media. Delivery is flexible in terms of mode and timing. And the institution is now offering Certificates of Advance Study (15-credit programs) in Cybersecurity, Human Resource Management and Project Management to meet the stated needs of our business partners seeking to upskill their employees.
Looking Ahead
Some of these changes and investments align with challenges identified before the pandemic as necessary if higher education institutions are to survive and sustain changing demographic and economic trends. The pandemic provided the opportunity to focus on these more quickly, allowing institutions such as Thomas College to right the ship today and set the right course for tomorrow.
Ed Cervone is vice president of innovative partnerships and the executive director of the Center for Innovation in Education at Thomas College, in Waterville, Maine., also the home of Colby College.
David Warsh: The mysterious machinery of epidemic models
“The Plague of Athens ‘‘ by Michiel Sweerts (painted in 1652-54), illustrating the devastating epidemic that struck Athens in 430 B.C., as described by the historian Thucydides.
SOMERVILLE, Mass.
It is not difficult to identify a 9/11 moment in the 2020 COVID-19 pandemic, an event after which everything changed. Until mid-March, politicians in Britain and the United States were cautiously optimistic. Prime Minister Boris Johnson advised, “We should all basically just go about our normal daily lives.” President Trump, in an Oval Office address on March 11, said that for the vast majority of Americans, the risk is very, very low.”
Five days later, on March 16, the British government took the first of a series of measures leading to a lockdown on March 23. On March 17, President Trump read a statement to a press briefing:
My administration is recommending that all Americans, including the young and healthy, work to engage in schooling from home when possible. Avoid gathering in groups of more than 10 people. Avoid discretionary travel. And avoid eating and drinking at bars, restaurants and public food courts. If everyone makes this change or these critical changes and sacrifices now, we will rally together as one nation and we will defeat the virus. And we’re going to have a big celebration all together. With several weeks of focused action, we can turn the corner and turn it quickly.
What happened? Imperial College, London, released a model-based study on March 16 that made headlines around the world, predicting as many as 2.2 million deaths might occur in the U.S., and 510,000 in the U.K. as a result of the pandemic. To this point, 265,000 US deaths have been reported, and another 58,030 in Britain.
Since March, economists have gone to work seeking to better understand the machinery of epidemiological models and the theories on which they are based. In “An Economist’s Guide to Epidemiology Models of Infectious Disease,” in the Journal of Economic Perspectives, Fall 2020, Christopher Avery, William Bossert, Adam Clark, Glenn Ellison and Sarah Fisher Ellison lay out the facts above, along with some of their findings.
Epidemiology has become more empirical over time, they say, and epidemiologists are learning to add parameters to their models. But they make less of a distinction between theory and empirical approaches than do economists. Meanwhile, “a model which posits a symmetric, bell-shaped evolution of cases over time cannot accommodate repeated changes in the rate of spread due to changing regulations, changing public perception, and ‘quarantine fatigue.’”
Not surprisingly, economists have begun looking for means of suppressing the virus by changing behaviors in manners as cost-effective as possible. Representative is James Stock, of Harvard University, who argued in September that lockdowns are too are too blunt a method to rely on in most cases. In “Policies for a Second Wave,” for a special summer edition of Brookings Papers on Economic Activity, Stock and David Baqaee, Emmanuel Farhi and Michael Mina proposed framing the wearing of masks as a patriotic duty, pursuing cheap and rapid testing, stressing contact tracing and quarantine, and implementing waste-water testing as a means of surveillance once the virus is suppressed.
Epidemiology is not the only discipline to come under economists’ lens. Bruce Sacerdote, Ranjan Schgal and Molly Cook ask Why Is All Covid-19 News Bad News? in a National Bureau of Economic Research working paper out this month. They fault mainstream media for underplaying news of vaccine trials and school re-openings. Ninety-one percent of articles by U.S. major media outlets have been negative in tone since the first of the year compared with 54 percent abroad and 65 percent in scientific journals. Stories discussing Donald Trump and hydroxychloroquine were more numerous than all stories combined about companies and individuals working on a vaccine, they complained.
Of course those stories about hydroxychloroquine may have been more about the nature of the president’s leadership than about COVID-19. Even so, there is indeed evidence of hierarchy and momentum in the reporting: what Wall Street Journal columnist Holman Jenkins, Jr. goes on about. It’s going to be a long time before the strange coincidence of Donald Trump and the virus is untangled. Integrated assessment of the pandemic has far to go.
David Warsh, a veteran columnist and an economic historian, is proprietor of economicprincipals.com, where this piece first ran.
Rachana Pradhan: How big pharma money colors Operation Warp Speed
April 16 was a big day for Moderna, the Cambridge, Mass., Massachusetts biotech company on the verge of becoming a front-runner in the U.S. government’s race for a coronavirus vaccine. It had received roughly half a billion dollars in federal funding to develop a COVID shot that might be used on millions of Americans.
Thirteen days after the massive infusion of federal cash — which triggered a jump in the company’s stock price — Moncef Slaoui, a Moderna board member and longtime drug-industry executive, was awarded options to buy 18,270 shares in the company, according to Securities and Exchange Commission filings. The award added to 137,168 options he’d accumulated since 2018, the filings show.
It wouldn’t be long before President Trump announced Slaoui as the top scientific adviser for the government’s $12 billion Operation Warp Speed program to rush COVID vaccines to market. In his Rose Garden speech on May 15, Trump lauded Slaoui as “one of the most respected men in the world” on vaccines.
The Trump administration relied on an unusual maneuver that allowed executives to keep investments in drug companies that would benefit from the government’s pandemic efforts: They were brought on as contractors, doing an end run around federal conflict-of-interest regulations in place for employees. That has led to huge potential payouts — some already realized, according to a KHN analysis of SEC filings and other government documents.
Slaoui owned 137,168 Moderna stock options worth roughly $7 million on May 14, one day before Trump announced his senior role to help shepherd COVID vaccines. The day of his appointment, May 15, he resigned from Moderna’s board. Three days later, on May 18, following the company’s announcement of positive results from early-stage clinical trials, the options’ value shot up to $9.1 million, the analysis found. The Department of Health and Human Services said that Slaoui sold his holdings May 20, when they would have been worth about $8 million, and will donate certain profits to cancer research. Separately, Slaoui held nearly 500,000 shares in GlaxoSmithKline, where he worked for three decades, upon retiring in 2017, according to corporate filings.
Carlo de Notaristefani, an Operation Warp Speed adviser and former senior executive at Teva Pharmaceuticals, owned 665,799 shares of the drug company’s stock as of March 10. While Teva is not a recipient of Warp Speed funding, Trump promoted its antimalarial drug hydroxychloroquine as a COVID treatment, even with scant evidence that it worked. The company donated millions of tablets to U.S. hospitals and the drug received emergency use authorization from the Food and Drug Administration in March. In the following weeks, its share price nearly doubled.
Two other Operation Warp Speed advisers working on therapeutics, Drs. William Erhardt and Rachel Harrigan, own financial stakes of unknown value in Pfizer, which in July announced a $1.95 billion contract with HHS for 100 million doses of its vaccine. Erhardt and Harrigan were previously Pfizer employees.
“With those kinds of conflicts of interest, we don’t know if these vaccines are being developed based on merit,” said Craig Holman, a lobbyist for Public Citizen, a liberal consumer advocacy group.
An HHS spokesperson said the advisers are in compliance with the relevant federal ethical standards for contractors.
These investments in the pharmaceutical industry are emblematic of a broader trend in which a small group with the specialized expertise needed to inform an effective government response to the pandemic have financial stakes in companies that stand to benefit from the government response.
Slaoui maintained he was not in discussions with the federal government about a role when his latest batch of Moderna stock options was awarded, telling KHN he met with HHS Secretary Alex Azar and was offered the position for the first time May 6. The stock options awarded in late April were canceled as a result of his departure from the Moderna board in May, he said. According to the KHN analysis of his holdings, the options would have been worth more than $330,000 on May 14.
HHS declined to confirm that timeline.
The fate of Operation Warp Speed after President-elect Biden takes office is an open question. While Democrats in Congress have pursued investigations into Warp Speed advisers and the contracting process under which they were hired, Biden hasn’t publicly spoken about the program or its senior leaders. Spokespeople for the transition didn’t respond to a request for comment.
The four HHS advisers were brought on through a National Institutes of Health contract with consulting firm Advanced Decision Vectors, so far worth $1.4 million, to provide expertise on the development and production of vaccines, therapies and other COVID products, according to the federal government’s contracts database.
Slaoui’s appointment in particular has rankled Democrats and organizations such as Public Citizen. They say he has too much authority to be classified as a consultant. “It is inevitable that the position he is put in as co-chair of Operation Warp Speed makes him a government employee,” Holman said.
The incoming administration may have a window to change the terms under which Slaoui was hired before his contract ends, in March. Yet making big changes to Operation Warp Speed could disrupt one of the largest vaccination efforts in history while the American public anxiously awaits deliverance from the pandemic, which is breaking daily records for new infections. Warp Speed has set out to buy and distribute 300 million doses of a COVID vaccine, the first ones by year’s end.
“By the end of December we expect to have about 40 million doses of these two vaccines available for distribution,” Azar said Nov. 18, referring to front-runner vaccines from Pfizer and Moderna.
Azar maintained that Warp Speed would continue seamlessly even with a “change in leadership.” “In the event of a transition, there’s really just total continuity that would occur,” the secretary said.
Pfizer, which didn’t receive federal funds for research but secured the multibillion-dollar contract under Warp Speed, on Nov. 20 sought emergency authorization from the FDA; Moderna just announced that it would do so. In total, Moderna received nearly $1 billion in federal funds for development and a $1.5 billion contract with HHS for 100 million doses.
While it’s impossible to peg the precise value of Slaoui’s Moderna holdings without records of the sale transactions, KHN estimated their worth by evaluating the company’s share prices on the dates he received the options and the stock’s price on several key dates — including May 14, the day before his Warp Speed position was announced, and May 20.
However, the timing of Slaoui’s divestment of his Moderna shares — five days after he resigned from the company’s board — meant that he did not have to file disclosures with the SEC confirming the sale, even though he was privy to insider information when he received the stock options, experts in securities law said. That weakness in securities law, according to good-governance experts, deprives the public of an independent source of information about the sale of Slaoui’s stake in the company.
“You would think there would be kind of a one-year continuing obligation [to disclose the sale] or something like that,” said Douglas Chia, president of Soundboard Governance and an expert on corporate governance issues. “But there’s not.”
HHS declined to provide documentation confirming that Slaoui sold his Moderna holdings. His investments in London-based GlaxoSmithKline — which is developing a vaccine with French drugmaker Sanofi and received $2.1 billion from the U.S. government — will be used for his retirement, Slaoui has said.
“I have always held myself to the highest ethical standards, and that has not changed upon my assumption of this role,” Slaoui said in a statement released by HHS. “HHS career ethics officers have determined my contractor status, divestures and resignations have put me in compliance with the department’s robust ethical standards.”
Moderna, in an earlier statement to CNBC, said Slaoui divested “all of his equity interest in Moderna so that there is no conflict of interest” in his new role. However, the conflict-of-interest standards for Slaoui and other Warp Speed advisers are less stringent than those for federal employees, who are required to give up investments that would pose a conflict of interest. For instance, if Slaoui had been brought on as an employee, his stake from a long career at GlaxoSmithKline would be targeted for divestment.
Instead, Slaoui has committed to donating certain GlaxoSmithKline financial gains to the National Institutes of Health.
Offering Warp Speed advisers contracts might have been the most expedient course in a crisis.
“As the universe of potential qualified candidates to advise the federal government’s efforts to produce a COVID-19 vaccine is very small, it is virtually impossible to find experienced and qualified individuals who have no financial interests in corporations that produce vaccines, therapeutics, and other lifesaving goods and services,” Sarah Arbes, HHS’s assistant secretary for legislation and a Trump appointee, wrote in September to Rep. James Clyburn (D.-S.C.), who leads a House oversight panel on the coronavirus response.
That includes multiple drug-industry veterans working as HHS advisers, an academic who’s overseeing the safety of multiple COVID vaccines in clinical trials and sits on the board of Gilead Sciences, and even former government officials who divested stocks while they were federal employees but have since joined drug company boards.
Dr. Scott Gottlieb and Dr. Mark McClellan, former FDA commissioners, have been visible figures informally advising the federal response. Each sits on the board of a COVID vaccine developer.
After leaving the FDA in 2019, Gottlieb joined Pfizer’s board and has bought 4,000 of its shares, at the time worth more than $141,000, according to SEC filings. As of April, he had additional stock units worth nearly $352,000 that will be cashed out should he leave the board, according to corporate filings. As a board member, Gottlieb is required to own a certain number of Pfizer shares.
McClellan has been on Johnson & Johnson’s board since 2013 and earned $1.2 million in shares under a deferred-compensation arrangement, corporate filings show.
The two also receive thousands of dollars in cash fees annually as board members. Gottlieb and McClellan frequently disclose their corporate affiliations, but not always. Their Sept. 13 Wall Street Journal op-ed on how the FDA could grant emergency authorization of a vaccine identified their FDA roles and said they were on the boards of companies developing COVID vaccines but failed to name Pfizer and Johnson & Johnson. Both companies would benefit financially from such a move by the FDA.
“It isn’t a lower standard for FDA approval,” they wrote in the piece. “It’s a more tailored, flexible standard that helps protect those who need it most while developing the evidence needed to make the public confident about getting a Covid-19 vaccine.”
About the inconsistency, Gottlieb wrote in an email to KHN: “My affiliation to Pfizer is widely, prominently, and specifically disclosed in dozens of articles and television appearances, on my Twitter profile, and in many other places. I mention it routinely when I discuss Covid vaccines and I am proud of my affiliation to the company.”
A spokesperson for the Duke-Margolis Center for Health Policy, which McClellan founded, noted that other Wall Street Journal op-eds cited his Johnson & Johnson role and that his affiliations are mentioned elsewhere. “Mark has consistently informed the WSJ about his board service with Johnson & Johnson, as well as other organizations,” Patricia Shea Green said.
Johnson & Johnson’s vaccine is in phase 3 clinical trials and could be available in early 2021.
Still, while they worked for the FDA, Gottlieb and McClellan were subject to federal restrictions on investments and protections against conflicts of interest that aren’t in place for Warp Speed advisers.
According to the financial disclosure statements they signed with HHS, the advisers are required to donate certain stock profits to the NIH — but can do so after the stockholder dies. They can keep investments in drug companies, and the restrictions don’t apply to stock options, which give executives the right to buy company shares in the future.
“This is a poorly drafted agreement,” said Jacob Frenkel, an attorney at Dickinson Wright and former SEC lawyer, referring to the conflict-of-interest statement included in the NIH contract with Advanced Decision Vectors, the Warp Speed advisers’ employing consulting firm. He said documents could have been “tighter and clearer in many respects,” including prohibiting the advisers from exercising their options to buy shares while they are contractors.
De Notaristefani stepped down as Teva’s executive vice president for global operations in October 2019, but according to corporate filings he would remain with the company until the end of June 2020 in order to “ensure an orderly transition.” He’s been working with Warp Speed since at least May overseeing manufacturing, according to an HHS spokesperson.
When Erhardt left Pfizer in May, U.S. COVID infections were climbing and the company was beginning vaccine clinical trials. Erhardt and Harrigan, whose LinkedIn profile says she left Pfizer in 2010, have worked as drug industry consultants.
“Ultimately, conflicts of interest in ethics turn on the mindset behavior of the responsible persons,” said Frenkel, the former SEC attorney. “The public wants to know that it can rely on the effectiveness of the therapeutic or diagnostic product without wondering if a recommendation or decision was motivated for even the slightest reason other than product effectiveness and public interest.”
Rachana Pradhan is a Kaiser Health News correspondent.
Looking across the Charles River toward Kendall Square, Cambridge, headquarters of Moderna and other tech companies.
Philip K. Howard: Principles to unify America
The Great Seal of the United States. The Latin means “Out of Many, One’’
“America is deeply divided”: That’s the post-mortem wisdom from this year’s election.
Surveys repeatedly show, however, that most Americans share the same core values and goals, such as responsibility, accountability and fairness. One issue that enjoys overwhelming popular support is the need to fix broken government. Two-thirds of Americans in a 2019 University of Chicago/AP poll agreed that government requires “major structural changes.”
President-elect Biden has a unique opportunity to bring Americans together by focusing on making government work better. Extremism is an understandable response to the almost perfect record of public failures in recent years. The botched response to COVID-19, and continued confusion over imposing a mask mandate, are just the latest symptoms of a bureaucratic megalith that can’t get out of its own way. Almost a third of the health-care dollar goes to red tape. The United States is 55th in World Bank rankings for ease of starting a business. The human toll of all this red tape is reflected in the epidemic of burnout in hospitals, schools, and government itself.
More than anything, Washington needs a spring cleaning. Officials and citizens must have room to ask: “What’s the right thing to do here?” If we want schools and hospitals to work, and for permits to be given in months instead of years, Americans at every level of responsibility must be liberated to use their common sense. Accountability, not suffocating legal dictates, should be our protection against bad choices.
But there’s a reason why neither party presented a reform vision: It can’t be done without cleaning out codes that are clogged with interest-group favors. Changing how government works is literally inconceivable to most political insiders. I remember the knowing smile of then-House Speaker John Boehner’s (R.-Ohio) when I suggested a special commission to clean out obsolete laws, such as the 1920 Jones Act, which, by forbidding foreign-flag ships from transporting goods between domestic ports, can double the cost of shipping. I also remember the matter-of-fact rejection by then-Rep. Rahm Emanuel (D.-Ill.) of pilot projects for expert health courts — supported by every legitimate health-care constituency, including AARP and patient groups — when he heard that the National Trial Lawyers opposed it: “But that’s where we get our funding.”
Cleaning the stables would help everyone, but the politics of incremental reform are insurmountable. That’s why, as with closing unnecessary defense bases, the only path to success is to appoint independent commissions to propose simplified structures. Then interest groups and the public at large can evaluate the overall benefits of the new frameworks.
Over the summer, 100 leading experts and citizens, including former governors and senators from both parties, launched a Campaign for Common Good calling for spring cleaning commissions. Instead of thousand-page rulebooks, the Campaign proposed that new codes abide by core governing principles, more like the Constitution, that honor the freedom of citizens and officials alike to use their common sense:
Six Principles to Make Government Work Again
Govern for Goals. Government must focus on results, not red tape. Simplify most law into legal principles that give officials and citizens the duty of meeting goals, and the flexibility to allow them to use their common sense.
Honor Human Responsibility. Nothing works unless a person makes it work. Bureaucracy fails because it suffocates human initiative with central dictates. Give us back the freedom to make a difference.
Everyone is Accountable. Accountability is the currency of a free society. Officials must be accountable for results. Unless there’s accountability all around, everyone will soon find themselves tangled in red tape.
Reboot Regulation. Too few government programs work as intended. Many are obsolete. Most squander public and private resources with bureaucratic micromanagement. Rebooting old programs will release vast resources for current needs such as the pandemic, infrastructure, climate change, and income stagnation.
Return Government to the People. Responsibility works for communities as well as individuals. Give localities and local organizations more ownership and control of social services, including, especially, for schools and issues such as homelessness.
Restore the Moral Basis of Public Choices. Public trust is essential to a healthy culture. This requires officials to adhere to basic moral values — especially truthfulness, the golden rule, and stewardship for the future. All laws, programs and rights mist be justified for the common good. No one should have rights superior to anyone else.
Is America divided? Many of the problems that caused people to take to the streets this year reflect the inability of officials to act on these principles. The cop involved in the killing of George Floyd should have been taken off the streets years ago — but union rules made accountability impossible. The delay in responding to COVID was caused in part by ridiculous red tape. The inability to build fire breaks on the west coast was caused by procedures that disempowered forestry officials.
The enemy is not each other, as President-elect Biden has repeatedly said. The enemy is the Washington status quo — a ruinously expensive and paralytic bureaucratic quicksand. Change is in the air. But the politics are impossible. That’s why one of first acts of President Biden should be to appoint spring cleaning commissions to propose new frameworks that will liberate Americans at all levels of responsibility to roll up their sleeves and make America work again.
American government needs big change, but the changes could hardly be less revolutionary. Instead of attacking each other, Americans need to unite around core values of responsibility and good sense.
Philip K. Howard is founder of Campaign for Common Good. His latest book is Try Common Sense. Follow him on Twitter: @PhilipKHoward.
Mr. Howard, a lawyer, is the founder and chairman of the nonprofit legal- and regulatory-reform organization Common Good (commongood.org), a New York City-based civic and cultural leader and a photographer. This piece first ran in The Hill.
Chris Powell: Deconstructing COVID-19 hysteria
“Hysteria Patient,’’ by Andre Brouillet (1857-1914)
MANCHESTER, Conn.
Amid the growing panic fanned by news organizations about the rebound in the virus epidemic, last week's telling details were largely overlooked.
First, most of the recent "virus-associated" deaths in Connecticut again have been those of frail elderly people in nursing homes.
Second, while dozens of students at the University of Connecticut at Storrs recently were been found infected, most showed no symptoms and none died or was even hospitalized. Instead all were waiting it out or recovering in their rooms or apartments.
And third, the serious-case rate -- new virus deaths and hospitalizations as a percentage of new cases -- was running at about 2 percent, a mere third of the recent typical "positivity" rate of new virus tests, the almost meaningless detail that still gets most publicity.
Recognizing that deaths, hospitalizations, and hospital capacity should be the greatest concerns, Connecticut Gov. Ned Lamont last week recalled that at the outset of the epidemic he had the Connecticut National Guard erect field hospitals around the state and that 1,700 additional beds quickly became available but were never used. This option remains available.
The governor's insight should compel reflection about state government's policy on hospitals -- policy that for nearly 50 years has been, like the policy of most other states, to prevent their increase and expansion.
The premise has been the fear that, as was said in the old movie, "if you build it, they will come" -- more patients, that is. The demand for medical services, the policy presumes, is infinite, and since government pays most medical costs directly or indirectly, services must be discreetly rationed -- that is, without public understanding -- even if this prevents economic competition among medical providers.
So in Connecticut and most other states you can't just build and open a hospital; state government must approve and confer a "certificate of need." Who determines need? State government, not people seeking care.
Of course, this policy was not adopted with epidemics in mind. Indeed, in adopting this policy government seems to have thought that epidemics were vanquished forever by the polio vaccines in the 1960s.
Now it may be realized that, while epidemics can be exaggerated, as the current one is, they have not been vanquished and the current epidemic -- or, rather, government's response to it -- has crippled the economy, probably in the amount of billions of dollars in Connecticut alone.
That cost should be weighed against the cost of hospitals that were never built. Maybe they could have been built and maintained only for emergency use, and an auxiliary medical staff maintained too, just as the National Guard is an all-purpose auxiliary.
Also worth questioning is the growing clamor for virus testing. The heightened desire for testing in advance of holiday travel is natural, but testing is not so reliable, full of false positives and negatives. Someone can test negative on Monday and on Tuesday can start manifesting the virus or contract it and be without symptoms.
Testing may be of limited use for alerting people that they might well isolate themselves for a time even if they are without symptoms. But people without symptoms are far less likely to spread the virus than infected people who don't feel well.
Only daily testing of everyone might be reliable enough to be very effective, but government and medicine are not equipped for that and it would be impractical anyway. Weekly testing of all students and teachers in school might be practical and worthwhile but terribly expensive, and only a few wealthy private schools are attempting it.
Contact tracing policy needs revision. Nothing has been more damaging and ridiculous than the closing of whole schools for a week or more because one student or teacher got sick or tested positive. As the governor notes, because of their low susceptibility to the virus, children may be safer in school than anywhere else.
Risk for teachers is higher but they also are more likely to become infected outside of school. They might accept the risk in school out of duty to their students, whose interrupted education is the catastrophe of the epidemic.
Meanwhile the country needs two vaccines -- one against the virus itself and one against virus hysteria.=
Chris Powell is a columnist for the Journal Inquirer, in Manchester, Conn.
Llewellyn King: Trust deficit endangers vaccine rollout
An anti-vaccination caricature by James Gillray, “The Cow-Pock—or—The Wonderful Effects of the New Inoculation!’’ (1802)
WEST WARWICK, R.I.
There is a trust deficit in this country, and it may kill a lot of us.
We haven’t been trusting for a long time, but distrust reached its zenith during and after the recent election. The election, still contested, brought with it a massive overhang of distrust. Indeed, the past four years have been marked by wide distrust.
Distrusting the election results isn’t fatal. But distrusting the experts on the need to get vaccinated for COVID-19 is. Yet there are reports that as many as 50 percent of Americans won’t get the vaccine when it is available. That is lethal and a true threat to national security, the economy, our way of life, everything.
If we don’t get our jabs, we will continue to die from coronavirus at an alarming rate. Over 258,000 Americans have perished and the Centers for Disease Control and Prevention projects 298,000 deaths by mid-December.
As I recall, it was during the late 1960s that we began wide distrusting. By the end of the Vietnam War, we distrusted on a huge scale. We distrusted what we were told by the military, what we were told by President Lyndon Johnson and then by President Richard Nixon.
We also distrusted the experts. Just about all experts on all subjects, from nuclear-power safety to the environmental impact of the Concorde supersonic passenger jet.
Beyond Vietnam, distrust was fed by the unfolding evidence that we had been the victims of systemic lying. This led to big social realignments, as seen in the civil rights movement, the women’s movement, and the environmental movement. These betrayals exacerbated our natural American distrust of officialdom.
The establishment and its experts had been caught lying about the war and about other things. It was a decade that detonated trust, shredded belief in expertise, and left many of us feeling that we might as well make it up as we went along.
Now the trust deficit is back.
If LBJ and Nixon fueled distrust in the 1960s and early 1970s, the current breach of trust belongs to President Trump and his enablers scattered across the body politic, from presidential counselor Kellyanne Conway with her “alternative facts” to the Senate Republicans and their disinclination to check the president.
The trust deficit has divided us. Seventy-three million did vote for Trump and many of those believe what, most dangerously, he has said about the pandemic.
The result has been the growth of diabolical myths about COVID-19. Taking seriously some, or all, of Trump’s outpourings on the coronavirus -- from his advocacy of sunlight and his off-label drug recommendations, such as hydroxychloroquine, to putting the pandemic out of mind as a “hoax” -- fomented its spread.
We have been waiting for a medical breakthrough to repel and conquer COVID-19 and it looks as though that is at hand with the arrival of not one but three vaccines, the first of which should be available in about three weeks to the most vulnerable populations. The development of these vaccines represents a stupendous medical effort: the Manhattan Project of medicine.
But it will all be in vain if Americans don’t trust the authorities and don’t get vaccinated. It looks as though, according to surveys, 50 percent of the population will get vaccinated. The rest will choose to believe in such medical fictions as herd immunity — a pernicious idea that eventually we will all be immune by living with COVID-19. It should be noted that this didn’t happen with such other infectious diseases as bubonic plague, smallpox, polio, even the flu.
My informal survey of research doctors puts the odds on who will get vaccinated a little better than 50 percent. They conclude that one third will get vaccinated, one third will wait to see the results among those who got vaccinated early, and one third won’t get vaccinated, believing that the disease has been hyped and that it isn’t as serious as the often-castigated media says. Some of the “COVID-19 deniers” will be the permanent anti-vaxxers, people who think that vaccines have bad side effects; they believe, for example, that the MMR vaccine causes autism.
This medical heresy even as hospitals are filling to capacity, their staff are exhausted, and bodies are piling up in refrigerated trailers because there is nowhere to put them.
Without near-universal vaccination, the coronavirus will be around for years. The superhuman effort to get a vaccine will have been partially in vain. The silver bullet will be tarnished.
Get a grip, America. Get your jabs.
Llewellyn King is executive producer and host of White House Chronicle, on PBS. His email is llewellynking1@gmail.com. and he’s based in Rhode Island and Washington, D.C.
Before the anti-vaxxers: Administration of the polio inoculation, including by the first polio-vaccine developer, Jonas Salk, himself, in 1957 at the University of Pittsburgh, where his team had developed the vaccine.
In a postwar poster the Ministry of Health urged British residents to immunize children against diphtheria.
Karen Gross: Role-modeling by adults too often lacking in COVID-19 crisis
The Rev. John Jenkins, the president of the University of Notre Dame. Did he not wear a mask at a reception in order to suck up to Donald Trump?
BOSTON
From The New England Journal of Higher Education, a service of The New England Board of Higher Education (nebhe.org)
Sadly, the number of COVID-19 cases across the globe is rising. And while vaccines are in the offing, we may have many weeks between now and their availability, time in which more individuals can become infected and too many will die. In absolute terms, the numbers are staggering in the U.S. and around the world.
It is against this background that we should be concerned about super-spreader events. One category of such events includes college and high school students gathering and partying in ways that violate the COVID-19 protective measures (mask wearing, social distancing, avoiding large indoor get-togethers). Some of these problematic events occur off campus, others occur on campus. Wherever they happen, they have produced varying outcomes: quarantines; stoppage of athletic events; elimination of on-campus in-person learning (for a short or long period); changes in scheduling to eradicate vacations or campus departures; and students contracting COVID.
It is easy to blame students (whether in college or high school) and parents (in the context of high schoolers and even some college students who are now at home taking online classes). Can you hear adults within families and educational institutions saying: “How stupid can these young people be? They aren’t complying with the three simple rules.”
But the failure of compliance among young people must be contextualized. We are not living in “normal” times and behaviors need to be understood in light of the impact of the pandemic constraints as well as the age of students and their developmental stage.
Lack of physical connection, risk-taking, brain development
Start with this obvious observation: The wearing of masks, social distancing and school closures have left many young people without quality means of connecting. As much as they can use technology and we are certainly doing that (Zoom fatigue is a known phenomenon, as is online oversharing), there is something that youth are missing: real, hands-on human engagement. They are missing contact; they are missing touch. They are without smiles and hugs and physicality.
The absence of physical contact for an extended period (and what still seems like an indefinite period) is difficult and frustrating for young people. It makes them want to rebel against the constraints and ignore the accompanying risks that often are known to them. In short, students disobey COVID-19 rules because they have real needs for in-person connectivity that are unmet.
Brain science supports this conclusion: Most young people cannot fully control their behavior on their own and they discard the COVID-19 rules because of the stage of their brain development. Risk-taking is common among young people; it goes hand and hand with their psychosocial development. We know that young people underestimate risk: think about fast cars and drunk driving, texting while driving and physical challenges that seem likely to cause serious physical injury. Also, we know that quality judgment and decision-making do not occur until the mid to late 20s. (There are also upsides to this stage of development but that’s the subject of another article.)
Our expectation of strict compliance misses the biological reality of why students are disobeying. The parts of their brain that manage and measure risks are not fully developed. Youth are not trying to be disobedient (well, some are as a form of rebellion that is also age-appropriate). Many simply are not able to make quality decisions—at least not without adult intervention, and therein lie some answers as to what we can do to move toward greater compliance.
Two concrete examples
Before turning to solutions, let’s look at two actual scenarios that inform a pathway forward.
In late October, more than 20 high schoolers attended a party at a private home in Marblehead, Mass. Not only was there an absence of mask wearing, there was an absence of social distancing and there was shared drinking out of cups. The police were called. The students scattered. No one was prosecuted. The superintendent in a remarkably astute letter recognized student needs to connect, but then closed the high school as a precaution and decried that they can and must do better.
A few months earlier, Marist College, in Poughkeepsie, N.Y., suspended some students for participating in off-campus parties and later, when the non-compliance continued, had to shut down the campus physically. Before moving to online learning, the college president was quoted as saying: “Please don’t be a knucklehead who disregards the safety of others and puts our ability to remain on campus at risk.”
Pathways forward
We know that student risky behavior can be modified, and there are a variety of strategies that enable change. The problem is that we have not deployed them in the context of this pandemic for reasons that aren’t at all clear to me.
We would be wise to spend more time recognizing the psychological reasons for student behavior and, based on that science, create new strategies that mitigate the reasons noted above for non-compliance. And since the stage of student development also opens the door to creativity, why not use creativity as part of the solution?
Consider these approaches: Social-norming campaigns can show compliance or willingness to comply by many students to norms despite peer perceptions. Detailed discussions with students can lead to an understanding of the risks (based on science) to others and themselves with concrete examples and data points. Youth empathy engines can be activated such that students are engaged in doing activities that help others in their communities. These can be conducted by parents and educators alike. Consider a version of this “rock” project in Texas. Students could all get and paint rocks and then they and other students can place the rocks around school buildings or a college campus.
For the record, let’s eliminate one approach: student punishment and suspension as the first line of defense. We should be punishing when there is intent. Absent intent, we should not rush into suspending students. Yes, based on parties, we need to quarantine; yes, based on parties, we need to shut down campus residential life or in-person learning for a period of time. But calling people “knuckleheads” is not helpful.
Instead, let’s think about preemptive things that could be done to prevent the non-compliant risky behavior. We can do better, as the superintendent suggested, but we need to get ahead of the problem and not be reactive to it.
Role models
From my perspective, perhaps one of the best strategies for enabling students to shift behavioral patterns and avoid risky and unwise behavior is role modeling. We know that role modeling is critically important to youth. And role models can come from a variety of locations: family, older friends and peers, educators (including administrators and coaches), religious figures and community leaders. We also know that role models can be individuals whom students do not know personally: politicians, actors, athletes.
We know, too, that an antidote to trauma is a non-familial figure who knows you and genuinely cares about your well-being and believes in you. And we know that positive role models can and do counteract negative childhood and adult experiences. Our adults need to step it up—engage with one another and their children and peers in new ways.
Despite these truths, we aren’t doing a good job of role modeling locally or nationally. Consider the absence of good role modeling in the two concrete examples given earlier involving Marblehead and Marist and similar communities, schools and colleges.
With respect to Marblehead and similar communities where parties have occurred, I would ask (in a non-accusatory way): Where were the parents who lived in the home where the party was held? Were they home? Were they aware of the party in advance? Did they buy the items for the party? Where were the parents of the other students who attended the party? Did they know where their children were going that evening? What had the parents done in anticipation of the needs of their children to plan events that would be safe? What had the high school done in advance to recognize the need for students to engage but to construct initiatives that were safe for each student and the collective of students?
With respect to Marist and similar colleges, I would ask (again, in a non-accusatory way): Where were the student life personnel? Were they aware of particular off-campus sites that might present risks? What did they do in advance to provide for the engagement needs of students in safe ways? What messaging was coming from the administration in advance? And was the reference to the students as knuckleheads wise? By way of contrast, the superintendent in Marblehead overtly recognized the student need to engage in person in these difficult times, although for safety reasons, he closed in-person learning.
For me, Lesson One is that the institutions (both high school and postsecondary) and parents need to anticipate what activities could have meet student needs. And they should involve students in planning these events. There are a myriad of possibilities: art-installation projects; distant dancing; car get-togethers (remember “car hops?) with limited numbers in cars where students listen to live music or watch a movie together? What about wrapping all the trees in crepe paper to create a “Christo-esque” artwork and even, teaching about Christo and Jeanne-Claude’s amazing and startling work involving wrapping buildings and bridges and parks?
We can be creative in seeing what the needs are and then developing approaches that meet the needs.
Lesson Two is that the parents (of the party home) and the parents of other teenagers were not (it appears) actively aware of their own child’s behavior. Had they been, I think one can rightly ask whether they would have intervened. And we can rightly ask whether they themselves, in their engagement with others, were role modeling the needed protective behavior (masks, social distancing and outdoor events). Or perhaps they did not believe in the science and thus were noncompliant.
At the college level, I’d suggest there were staff who could have guessed where problems off-campus were likely, especially if they knew their students and had their ears to the ground. Even if this was not their role before and seems interventionist or paternalistic (maternalistic), that non-interference calculus has changed when there are abundant and growing health risks not just to students but to communities. Stated differently, why did staff not act on what they learned, knew and anticipated?
Both examples showcase the absence of role modeling by adults in terms of actual behavior and anticipatory thinking.
Negative role modeling is way too common right now
Apart from role modeling by parents and educators whom students know, we have had far too many examples of failed role modeling in ways that have received national attention. And, make no mistake about this, students are well aware when public figures fail to comply with the COVID mandates and rightly ask: If they can flaunt the rules, why can’t I?
Here are several well-known examples (and I am avoiding the obvious one of our current president) that demonstrate what students are seeing in the media day-in and day-out.
Start with the Dodgers Justin Turner’s behavior following his team winning the World Series. I get the excitement but having just tested positive, he went out onto the field maskless for at least some of the time. What message does that send to young people? When you win, the rules don’t apply even though the coach was among people who were immune-compromised? And then the player went unsanctioned by Major League Baseball as if the incident should just be forgotten as a lapse in a moment of glory and because the player issued an apology.
Turn then to Gavin Newsom, the governor of California, a state struggling with COVID outbreaks (among other disasters). It turns out that he attended a birthday party with more than 10 unrelated family members at an elite restaurant in Napa and wasn’t wearing a mask apparently. Top doctors attended, too. All of this was directly in contradiction to the mandates he was issuing to his constituencies.
But perhaps the most offensive examples come from college presidents. Think about it. If our educational leaders, who have a bully pulpit and are preaching compliance to their institutions, don’t comply, why would their students or students on other campuses? A prime example is Notre Dame’s president, the Rev. John Jenkins. He attended a ceremony in honor of the nomination of Amy Coney Barrett to the Supreme Court. To be sure, for his institution, this was a big deal as the nominee was a professor at Notre Dame’s Law School. But please, no mask? No social distancing? Was he afraid that the president (of the U.S) would see a mask as a sign of disrespect? The photographs of the non-compliance are chilling.
Students were rightfully angry as were faculty. An apology isn’t enough in the context of the virus; words don’t stop disease spread, especially when you are so forcefully asking for campus compliance with COVID protections. And Father Jenkins got COVID.
Lesson Three is obvious: Hypocrisy doesn’t fly in the COVID-19 world. Public high-profile leaders need to role model compliance all the time; their messaging is seen and heard and it matters. Negative role modeling is catching.
Now what?
The contents of this article and the examples given and lessons proffered boil down to this: We need to ramp up positive role modeling. Role modeling isn’t a part-time activity. It is a full-time obligation.
To that end, parents and educators: 1) need to come up with strategies in advance that recognize that young people need ways to engage safely; 2) must involve students in the planning of these activities that are COVID-safe; 3) need to question where students are and anticipate their behavior by offering alternatives; 4) need to talk more to students about risks and about solutions and about feelings and double standards; and 5) shouldn’t make punishment the best solution as it doesn’t work; instead, provide alternatives.
These aren’t impossible solutions. They are doable if we focus on them. And we should, for the well-being of our young people, our families and our communities.
Karen Gross is former president of Southern Vermont College and a senior policy adviser to the U.S. Department of Education. She specializes in student success and trauma across the educational landscape. Her book, Trauma Doesn’t Stop at the School Door: Solutions and Strategies for Educators, PreK-College, was released in June 2020 by Columbia Teachers College Press.
Charlotte Huff: In COVID crisis, 'unattended moral injury' to health-care workers
St. Vincent Hospital in Worcester
For Christina Nester, the pandemic lull in Massachusetts lasted about three months through summer into early fall. In late June, St. Vincent Hospital had resumed elective surgeries, and the unit the 48-year-old nurse works on switched back from taking care of only COVID-19 patients to its pre-pandemic roster of patients recovering from gallbladder operations, mastectomies and other surgeries.
That is, until October, when patients with coronavirus infections began to reappear on the unit and, with them, the fear of many more to come. “It’s paralyzing, I’m not going to lie,” said Nester, who’s worked at the Worcester hospital for nearly two decades. “My little clan of nurses that I work with, we panicked when it started to uptick here.”
Adding to that stress is that nurses are caught betwixt caring for the bedside needs of their patients and implementing policies set by others, such as physician-ordered treatment plans and strict hospital rules to ward off the coronavirus. The push-pull of those forces, amid a fight against a deadly disease, is straining this vital backbone of health providers nationwide, and that could accumulate to unsustainable levels if the virus’s surge is not contained this winter, advocates and researchers warn.
Nurses spend the most sustained time with a patient of any clinician, and these days patients are often very fearful and isolated, said Cynda Rushton, a registered nurse and bioethicist at Johns Hopkins University, in Baltimore.
“They have become, in some ways, a kind of emotional surrogate for family members who can’t be there, to support and advise and offer a human touch,” Rushton said. “They have witnessed incredible amounts of suffering and death. That, I think, also weighs really heavily on nurses.”
A study published this fall in the journal General Hospital Psychiatry found that 64 percent of clinicians working as nurses, nurse practitioners or physician assistants at a New York City hospital screened positively for acute distress, 53 percent for depressive symptoms and 40 percent for anxiety — all higher rates than found among physicians screened.
Researchers are concerned that nurses working in a rapidly changing crisis like the pandemic — with problems ranging from staff shortages that curtail their time with patients to enforcing visitation policies that upset families — can develop a psychological response called “moral injury.” That injury occurs, they say, when nurses feel stymied by their inability to provide the level of care they believe patients require.
Dr. Wendy Dean, co-founder of Moral Injury of Healthcare, a nonprofit organization based in Carlisle, Pa., said, “Probably the biggest driver of burnout is unrecognized unattended moral injury.”
In parts of the country over the summer, nurses got some mental-health respite when cases declined, Dean said.
“Not enough to really process it all,” she said. “I think that’s a process that will take several years. And it’s probably going to be extended because the pandemic itself is extended.”
Before the pandemic hit her Massachusetts hospital “like a forest fire” in March, Nester had rarely seen a patient die, other than someone in the final days of a disease like cancer.
Suddenly she was involved with frequent transfers of patients to the intensive-care unit when they couldn’t breathe. She recounts stories, imprinted on her memory: The woman in her 80s who didn’t even seem ill on the day she was hospitalized, who Nester helped transport to the morgue less than a week later. The husband and wife who were sick in the intensive care unit, while the adult daughter fought the virus on Nester’s unit.
“Then both parents died, and the daughter died,” Nester said. “There’s not really words for it.”
During these gut-wrenching shifts, nurses can sometimes become separated from their emotional support system — one another, said Rushton, who has written a book about preventing moral injury among health- care providers. To better handle the influx, some nurses who typically work in noncritical care areas have been moved to care for seriously ill patients. That forces them to not only adjust to a new type of nursing, but also disrupts an often-well-honed working rhythm and camaraderie with their regular nursing co-workers, she said.
At St. Vincent Hospital, the nurses on Nester’s unit were told one March day that the primarily post-surgical unit was being converted to a COVID unit. Nester tried to squelch fears for her own safety while comforting her COVID-19 patients, who were often elderly, terrified and sometimes hard of hearing, making it difficult to communicate through layers of masks.
“You’re trying to yell through all of these barriers and try to show them with your eyes that you’re here and you’re not going to leave them and will take care of them,” she said. “But yet you’re panicking inside completely that you’re going to get this disease and you’re going to be the one in the bed or a family member that you love, take it home to them.”
When asked if hospital leaders had seen signs of strain among the nursing staff or were concerned about their resilience headed into the winter months, a St. Vincent spokesperson wrote in a brief statement that during the pandemic “we have prioritized the safety and well-being of our staff, and we remain focused on that.”
Nationally, the viral risk to clinicians has been well documented. From March 1 through May 31, 6 percent of adults hospitalized were health-care workers, one-third of them in nursing-related occupations, according to data published last month by the Centers for Disease Control and Prevention.
As cases mount in the winter months, moral injury researcher Dean said, “nurses are going to do the calculation and say, ‘This risk isn’t worth it.’”
Juliano Innocenti, a traveling nurse working in the San Francisco area, decided to take off for a few months and will focus on wrapping up his nurse practitioner degree instead. Since April, he’s been seeing a therapist “to navigate my powerlessness in all of this.”
Innocenti, 41, has not been on the front lines in a hospital battling COVID-19, but he still feels the stress because he has been treating the public at an outpatient dialysis clinic and a psychiatric hospital and seen administrative problems generated by the crisis. He pointed to issues such as inadequate personal protective equipment.
Innocenti said he was concerned about “the lack of planning and just blatant disregard for the basic safety of patients and staff.” Profit motives too often drive decisions, he suggested. “That’s what I’m taking a break from.”
Building Resiliency
As cases surge again, hospital leaders need to think bigger than employee-assistance programs to backstop their already depleted ranks of nurses, Dean said. Along with plenty of protective equipment, that includes helping them with everything from groceries to transportation, she said. Overstaff a bit, she suggested, so nurses can take a day off when they hit an emotional cliff.
The American Nurses Association, the American Association of Critical-Care Nurses (AACN) and several other nursing groups have compiled online resources with links to mental health programs as well as tips for getting through each pandemic workday.
Kiersten Henry, an AACN board member and nurse practitioner in the intensive care unit at MedStar Montgomery Medical Center, in Olney, Md., said that the nurses and other clinicians there have started to gather for a quick huddle at the end of difficult shifts. Along with talking about what happened, they share several good things that also occurred that day.
“It doesn’t mean that you’re not taking it home with you,” Henry said, “but you’re actually verbally processing it to your peers.”
When cases reached their highest point of the spring in Massachusetts, Nester said there were some days she didn’t want to return.
“But you know that your friends are there,” she said. “And the only ones that really truly understand what’s going on are your co-workers. How can you leave them?”
Charlotte Huff is a Kaiser Health News reporter.
The lure of the local
Mr. McFeely ("Speedy Delivery"), in Mister Rogers' Neighborhood, leads a group to the post office to hand deliver their completed 2010 Census forms during the "Count Me In In 2010 Rally" in Homestead, Penn.
From Robert Whitcomb’s “Digital Diary,’’ in GoLocal24.com
Then there are other local glimmers of light. An example: In the past couple of weeks, some of our neighbors in Providence organized outdoor parties to honor a couple of friendly (including to dogs) and very reliable mailmen in our neighborhood who recently retired. It was a joy to see such benign civic activities bringing people together.
But events like this are less likely today in our dispersed, suburban/exurban society, in which interactions are increasingly on screens. We make fewer opportunities to do things together in person.
Consider that we don’t shop together as much. I thought of this the other week as I strolled around the little downtown of the town where I spent much of my boyhood. Back then, everyone went to the village’s locally owned grocery store (accurately called “Central Market” and smelling of ground coffee) and the town’s only drugstore, also locally owned. You’d bump into friends and neighbors there. Indeed, you’d make friends there.
Both have long since closed, succeeded by chain drugstores and chain supermarkets dispersed around the area. While many villagers a half century ago would walk to the downtown almost daily to shop, now pretty much everyone drives to wind-swept store parking lots.
I wonder if, when the COVID-19 crisis fades, whether pent-up demand for real, in-person interactions might help revive small downtowns. And after all, malls and big-box stores at the periphery of the old downtowns had been closing at a good clip before the virus in the Amazon avalanche.