And in our next Civil War?
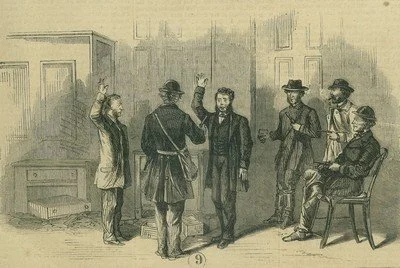
St. Albans , Vt., bank tellers being forced to pledge allegiance to the Confederacy on Oct. 19, 1864.
The St. Albans Raid, the northernmost land action of the American Civil War, was a raid from Canada by 21 Confederate soldiers. Their mission was to rob banks to raise money, and to trick the Union Army into diverting troops to defend their northern border against further raids. They got the money, killed a local and escaped back to Canada.
Charlotte Huff: In COVID crisis, 'unattended moral injury' to health-care workers
St. Vincent Hospital in Worcester
For Christina Nester, the pandemic lull in Massachusetts lasted about three months through summer into early fall. In late June, St. Vincent Hospital had resumed elective surgeries, and the unit the 48-year-old nurse works on switched back from taking care of only COVID-19 patients to its pre-pandemic roster of patients recovering from gallbladder operations, mastectomies and other surgeries.
That is, until October, when patients with coronavirus infections began to reappear on the unit and, with them, the fear of many more to come. “It’s paralyzing, I’m not going to lie,” said Nester, who’s worked at the Worcester hospital for nearly two decades. “My little clan of nurses that I work with, we panicked when it started to uptick here.”
Adding to that stress is that nurses are caught betwixt caring for the bedside needs of their patients and implementing policies set by others, such as physician-ordered treatment plans and strict hospital rules to ward off the coronavirus. The push-pull of those forces, amid a fight against a deadly disease, is straining this vital backbone of health providers nationwide, and that could accumulate to unsustainable levels if the virus’s surge is not contained this winter, advocates and researchers warn.
Nurses spend the most sustained time with a patient of any clinician, and these days patients are often very fearful and isolated, said Cynda Rushton, a registered nurse and bioethicist at Johns Hopkins University, in Baltimore.
“They have become, in some ways, a kind of emotional surrogate for family members who can’t be there, to support and advise and offer a human touch,” Rushton said. “They have witnessed incredible amounts of suffering and death. That, I think, also weighs really heavily on nurses.”
A study published this fall in the journal General Hospital Psychiatry found that 64 percent of clinicians working as nurses, nurse practitioners or physician assistants at a New York City hospital screened positively for acute distress, 53 percent for depressive symptoms and 40 percent for anxiety — all higher rates than found among physicians screened.
Researchers are concerned that nurses working in a rapidly changing crisis like the pandemic — with problems ranging from staff shortages that curtail their time with patients to enforcing visitation policies that upset families — can develop a psychological response called “moral injury.” That injury occurs, they say, when nurses feel stymied by their inability to provide the level of care they believe patients require.
Dr. Wendy Dean, co-founder of Moral Injury of Healthcare, a nonprofit organization based in Carlisle, Pa., said, “Probably the biggest driver of burnout is unrecognized unattended moral injury.”
In parts of the country over the summer, nurses got some mental-health respite when cases declined, Dean said.
“Not enough to really process it all,” she said. “I think that’s a process that will take several years. And it’s probably going to be extended because the pandemic itself is extended.”
Before the pandemic hit her Massachusetts hospital “like a forest fire” in March, Nester had rarely seen a patient die, other than someone in the final days of a disease like cancer.
Suddenly she was involved with frequent transfers of patients to the intensive-care unit when they couldn’t breathe. She recounts stories, imprinted on her memory: The woman in her 80s who didn’t even seem ill on the day she was hospitalized, who Nester helped transport to the morgue less than a week later. The husband and wife who were sick in the intensive care unit, while the adult daughter fought the virus on Nester’s unit.
“Then both parents died, and the daughter died,” Nester said. “There’s not really words for it.”
During these gut-wrenching shifts, nurses can sometimes become separated from their emotional support system — one another, said Rushton, who has written a book about preventing moral injury among health- care providers. To better handle the influx, some nurses who typically work in noncritical care areas have been moved to care for seriously ill patients. That forces them to not only adjust to a new type of nursing, but also disrupts an often-well-honed working rhythm and camaraderie with their regular nursing co-workers, she said.
At St. Vincent Hospital, the nurses on Nester’s unit were told one March day that the primarily post-surgical unit was being converted to a COVID unit. Nester tried to squelch fears for her own safety while comforting her COVID-19 patients, who were often elderly, terrified and sometimes hard of hearing, making it difficult to communicate through layers of masks.
“You’re trying to yell through all of these barriers and try to show them with your eyes that you’re here and you’re not going to leave them and will take care of them,” she said. “But yet you’re panicking inside completely that you’re going to get this disease and you’re going to be the one in the bed or a family member that you love, take it home to them.”
When asked if hospital leaders had seen signs of strain among the nursing staff or were concerned about their resilience headed into the winter months, a St. Vincent spokesperson wrote in a brief statement that during the pandemic “we have prioritized the safety and well-being of our staff, and we remain focused on that.”
Nationally, the viral risk to clinicians has been well documented. From March 1 through May 31, 6 percent of adults hospitalized were health-care workers, one-third of them in nursing-related occupations, according to data published last month by the Centers for Disease Control and Prevention.
As cases mount in the winter months, moral injury researcher Dean said, “nurses are going to do the calculation and say, ‘This risk isn’t worth it.’”
Juliano Innocenti, a traveling nurse working in the San Francisco area, decided to take off for a few months and will focus on wrapping up his nurse practitioner degree instead. Since April, he’s been seeing a therapist “to navigate my powerlessness in all of this.”
Innocenti, 41, has not been on the front lines in a hospital battling COVID-19, but he still feels the stress because he has been treating the public at an outpatient dialysis clinic and a psychiatric hospital and seen administrative problems generated by the crisis. He pointed to issues such as inadequate personal protective equipment.
Innocenti said he was concerned about “the lack of planning and just blatant disregard for the basic safety of patients and staff.” Profit motives too often drive decisions, he suggested. “That’s what I’m taking a break from.”
Building Resiliency
As cases surge again, hospital leaders need to think bigger than employee-assistance programs to backstop their already depleted ranks of nurses, Dean said. Along with plenty of protective equipment, that includes helping them with everything from groceries to transportation, she said. Overstaff a bit, she suggested, so nurses can take a day off when they hit an emotional cliff.
The American Nurses Association, the American Association of Critical-Care Nurses (AACN) and several other nursing groups have compiled online resources with links to mental health programs as well as tips for getting through each pandemic workday.
Kiersten Henry, an AACN board member and nurse practitioner in the intensive care unit at MedStar Montgomery Medical Center, in Olney, Md., said that the nurses and other clinicians there have started to gather for a quick huddle at the end of difficult shifts. Along with talking about what happened, they share several good things that also occurred that day.
“It doesn’t mean that you’re not taking it home with you,” Henry said, “but you’re actually verbally processing it to your peers.”
When cases reached their highest point of the spring in Massachusetts, Nester said there were some days she didn’t want to return.
“But you know that your friends are there,” she said. “And the only ones that really truly understand what’s going on are your co-workers. How can you leave them?”
Charlotte Huff is a Kaiser Health News reporter.
Some colleges must reopen by the fall or die
The former Southern Vermont College, in Bennington, closed last year. It’s one of several small New England colleges put out of business by changing student demographics. COVID-19 is likely to kill more of them in the coming months.
Adapted from Robert Whitcomb’s “Digital Diary,’’ in GoLocal24.com
Kudos to Brown University and some other schools that are making dorm rooms available to house front-line workers in the pandemic emergency. With large parts of these institutions effectively closed, they have plenty of space to offer.
But what happens next September? Many colleges and universities are now agonizing over whether COVID-19 will let them safely physically reopen. If not, how many students and their parents will be willing to spend tens of thousands of dollars to take classes via the likes of Zoom? The claims that online learning is almost as good as in-person classes are laughable. Zoom, Skype, et al., are technically impressive but frankly as a teaching vehicle they suck (to coin a phrase) compared to in-person instruction.
So I’d guess that many students will decide to take a “gap year,” with the idea of entering, or returning to, college in the fall of 2021. The trouble is that there won’t be many jobs available for them in the interim and that some of their colleges will die as the pandemic dries up their tuition and fees revenue.
It’s not clear how Trump’s latest immigration/foreign visitor orders might affect, at least indirectly, many foreign students at American colleges and universities, most paying full freight. The American Council on Education says that more than 1 million foreign students attend U.S. colleges and universities, contributing more than $39 billion to the economy and subsidizing American students.
In any case, a lot of these colleges must physically reopen by the fall or die.