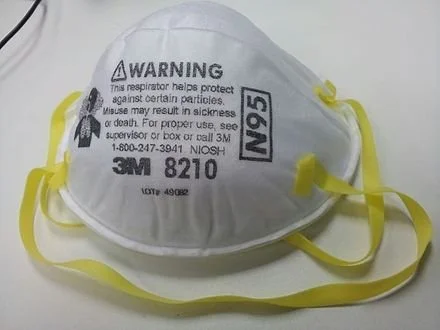
This N95 mask is highly effective.
— Photo by Banej
From Kaiser Health News in cooperation with PolitiFact
“From the perspective of knowing how covid is transmitted, and what we know about omicron, wearing a higher-quality mask is really critical to stopping the spread of omicron.’’
— Dr. Megan Ranney, academic dean for the School of Public Health at Brown University.
The highly transmissible omicron variant is sweeping the U.S., causing a huge spike in COVID-19 cases and overwhelming many hospital systems. Besides urging Americans to get vaccinated and boosted, public health officials are recommending that people upgrade from their cloth masks to higher-quality medical-grade masks.
But what does this even mean?
At a recent Senate Health, Education, Labor and Pensions Committee hearing, top public health officials displayed different types of masking. Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention, wore what appeared to be a surgical mask layered under a cloth mask, while Dr. Anthony Fauci, chief medical adviser to the president, wore what looked like a KN95 respirator.
(Dr. Wakensky was formerly chief of the Division of Infectious Diseases at Massachusetts General Hospital and a professor of medicine at Harvard Medical School.)
Some local governments and other organizations are offering their own policies. Los Angeles County, for instance, will require as of Jan. 17 that employers provide N95 or KN95 masks to employees. In late December, the Mayo Clinic began requiring all visitors and patients to wear surgical masks instead of cloth versions. The University of Arizona has banned cloth masks and asked everyone on campus to wear higher-quality masks.
Questions about the level of protection against COVID that masks provide — whether cloth, surgical or higher-end medical grade — have been a subject of debate and discussion since the earliest days of the pandemic. We looked into the question last summer. And as science changes and variants emerge with higher transmissibility, so do opinions.
The Centers for Disease Control and Prevention has not updated its mask guidance since October, before the omicron variant emerged. That guidance doesn’t recommend the use of an N95 respirator but states only that masks should be at least two layers, well-fitting and contain a nose wire.
Multiple experts we consulted said that the current CDC guidance does not go far enough. They also agreed on another point: Wearing a cloth mask is better than not wearing a mask at all, but if you can upgrade — or layer cloth with surgical — now is the time.
Although cloth masks may appear to be more substantial than the paper surgical mask option, surgical masks as well as KN95 and N95 masks are infused with an electrostatic charge that helps filter out particles.
“From the perspective of knowing how COVID is transmitted, and what we know about omicron, wearing a higher-quality mask is really critical to stopping the spread of omicron,” said Dr. Megan Ranney, academic dean for the School of Public Health at Brown University.
A large-scale real-world study conducted in Bangladesh and published in December showed that surgical masks are more effective at preventing covid transmission than cloth masks.
So, one easy strategy to improve protection is to layer a surgical mask underneath cloth. Surgical masks can be bought relatively cheaply online and reused for about a week.
Ranney said she advises people who opt for layering to put the better-quality mask, such as the surgical mask, closest to your face, and put the lesser-quality mask on the outside.
If you’re really pressed for resources, Dr. Stephen Luby, a professor specializing in infectious diseases at Stanford University and one of the authors of the Bangladesh mask study, said surgical masks can be washed and reused, if finances are an issue. Nearly two years into the pandemic, such masks are cheap and plentiful in the U.S. and many retailers make them available free of charge to customers as they enter businesses.
“During the study, we told the participants they could wash the surgical masks with laundry detergent and water and reuse them,” Luby said. “You lose some effect of the electrostatic charge, but they still outperformed cloth masks.”
Still, experts maintain that wearing either a KN95 or an N95 respirator is the best protection against omicron, since these masks are highly effective at filtering out viral particles. The “95” in the names refers to the masks’ 95% filtration efficacy against certain-sized particles. N95 masks are regulated by the National Institute for Occupational Safety and Health, while KN95s are regulated by the Chinese government and KF94s by the South Korean government.
Americans were initially urged not to buy either surgical or N95 masks early in the pandemic to ensure there would be a sufficient supply for health care workers. But now there are enough to go around.
So, if you have the resources to upgrade to an N95, a KN95 or a KF94 mask, you should absolutely do so, said Dr. Leana Wen, a professor of health policy and management at George Washington University. Although these models are more expensive and can be more uncomfortable, they are worth the investment for the safety they provide, she said.
“[Omicron is] a much more contagious virus, so there is a much lower margin of error in regards to the activities you were once able to do without getting infected,” Wen said. “We have to increase our protection in every way, because everything is riskier now.”
Wen also said that though these masks are characterized as one-use, unless you are in a health care setting, KN95s and N95s can be worn more than once. She uses one of her personal KN95s for more than a week at a time.
Another important thing to note is there are many counterfeit N95 and KN95 masks being sold online, so consumers must be careful when ordering them and be sure to get them only from a legitimate, trusted vendor.
The CDC maintains a list of NIOSH-approved N95 respirators. Wirecutter and The Strategist have both published guides to purchasing approved KN95 and KF94 masks. Ranney also recommends consulting the website Project N95 or engineer Aaron Collins’s “Mask Nerd” YouTube channel.
And remember, the risk of transmission depends not just on the mask you wear but also the masking practices of others in the room — so going into a meeting or restaurant where others are unmasked or wearing only cloth masks increases the odds of getting infected, no matter how careful you are. This chart demonstrates the huge differences.
Even with a mask upgrade, if you are still worried about omicron and, in particular, a serious case of , the No. 1 thing you can do to protect yourself is get vaccinated and boosted, said Dr. Neal Chaisson, an assistant professor of medicine at the Cleveland Clinic.
“There’s been a lot of talk about people who have been vaccinated getting omicron,” said Chaisson. “But I’ve been working in the ICU and probably 95% of the patients that we’re taking care of right now did not take the advice to get vaccinated.”
Victoria Knight is a Kaiser Health News reporter
vknight@kff.org, @victoriaregisk